作者:
浏览量:55
日期:2025-07-21
Billingual Acupuncture and Moxibustion
Part Ⅱ Needling and Moxibustion Techniques
Chapter 4 General Introduction to Needling
and Moxibustion Techniques
4.1 Concepts and Functions of Needling and Moxibustion Techniques
Needling Techniques: This refers to the specific techniques and methods of stimulating certain parts of the body, using different needle or non-needle tools for the functions of the meridians and qi, to regulate the functions of the body.
Moxibustion Techniques: This refers to the use of heat stimulation on the surface of the body, generated by burning moxa, or in conjunction with other medicinal substances.
Functions of Needling and Moxibustion: They have the effects of dredging the channels and collaterals, regulating yin and yang in the internal organs and promoting the circulation of qi and blood via stimulation of certain parts of the body (acupoints), finally resulting in strengthening body resistance and eliminating evil in an overall effort to cure diseases.
4.2 Origin of Needling and Moxibustion Techniques
4.2.1 Origin and Development of Acupuncture Techniques
4.2.1.1 Origin of Acupuncture Techniques
The origin of acupuncture techniques can be traced back to the Neolithic Age. There are stone needles which are thought to be acupuncture and cutting tools (bianshi). The book of Shuo Wen Jie Zi explained that “bian ” means treating disease by using a stone. A small stone polished into a conical shape or wedge was used for bloodletting and cutting, for rubbing or rapping certain parts of the skin.
When people feel pain in somewhere of their body, they will naturally rub or thump the spot, to reduce or relieve the pain. Stone needle acupuncture was the predecessor of later acupuncture therapy. Besides stone needle, ancient needles were also made of bones, bamboo and ceramic.
4.2.1.2 Development of Needling Tools
Ancient—Bronze Age-Iron Age … The Development of Metallurgy—Modern Stone Needles, Bone Needles- Metal Needles (Bronze Needles), The Nine Needles in Huang Di Nei Jing—Gold Needles, Silver Needles, Alloy Needles, Stainless Steel Needles—Acupuncture Therapeutic Apparatus (Electric Acupuncture Apparatus, Acupuncture Manipulation Apparatus).
4.2.1.3 Development of Needling Techniques
If one observes the history of acupuncture instruments, there was a continuous improvement in acupuncture techniques. Nei Jing summarized the ancient acupuncture techniques and made a brilliant exposition. For needling techniques, the Nine Needling Techniques, the Twelve Needling Techniques and the Five Needling Techniques were mentioned. For the manipulation techniques, the Reinforcing and Reducing Methods of being rapid and slow (Xu Ji), inhalation and exhalation (Hu Xi), twirling and rotating (Nian Zhuan), directing (Ying Sui), lifting and thrusting (Ti Cha), and open-close (Kai He) were also recorded. Nan Jing developed needling techniques with special emphasis on the importance of the coordination between both hands. From the Jin and Tang Dynasties to the Song Dynasty, similar techniques in the Nei Jing and Nan Jing were used and discussed. Until the Jin and Yuan Dynasties, the Time Needling Technique of “midnight-noon and ebb-flow doctrine” was developed, a method of pointselection therapy based on the circulation time of qi and blood. Yang Ji-zhou of the Ming Dynasty summarized the essence of acupuncture manipulation before the Ming Dynasty, pointing out that there were strong or gentle needling techniques such as the drastic reinforcing or reducing method, the even method, in addition to the Twelve and Eight Techniques of Inserting Needles, which are all commonly used in the clinic practice. After the middle of the Qing Dynasty, there was a declination in the new development and innovation in acupuncture techniques.
A new period of great development occurred in the field of acupuncture academics, research and techniques after the 1950s. A great deal of work was conducted in literary investigations and clinical observations resulting in many achievements. At present, more attention is being paid to the traditional techniques. In addition, a new development on traditional techniques is combining acupuncture techniques with physical therapy and point injection therapy. Some therapeutic approaches put emphasis on point selections in local areas resulting in the development of auricular acupuncture and scalp acupuncture, etc.
4.2.2 Origin and Development of Moxibustion Techniques
4.2.2.1 Origin of Moxibustion Techniques
Acupuncture and Moxibustion in Chinese writing are written as 针灸 ( 针,means needle, 灸, composed of, 久, meaning long, 火, meaning fire). The practice went from natural fire to warmer stone, then to herb burning. Having a history even longer than acupuncture (especially in the north of China), moxibustion was the burning on the skin of herbal moxa at acupuncture points. The most popular material for moxibustion was the dried leaf of Artemisia Vulgaris (meaning common artemisia). It later became the thunder-fire moxibustion (lei huo zhen) and Taiyi moxa stick (taiyi shen zhen) which were made of moxa sticks mixed with medicamental pulverata and moxa. Modern application of moxibustion with sticks or herbal sticks is a further development of older methods.
It is also the combination of moxibustion and ironing methods.
4.2.2.2 Development of Moxibustion Techniques
In 1973, the earliest medical literature, a book written on silk, recording moxibustion, was unearthed in the tomb of Ma Wang Dui in Changsha.
Nei Jing recorded that the development of moxibustion had a close relationship with people’s living environment, their life habit and the property of the diseases. Nei Jing also recorded the indications and dosages, the order of moxibustion and reinforcing and reducing with moxibustion, and recommended using acupuncture and moxibustion in combination. Zhen Jiu Jia Yi Jing and Bei Ji Qian Jin Yao Fang vigorously advocated using
acupuncture and moxibustion in combination. In contrast, Wai Tai Mi Yao put the emphasis on moxibustion and gave up acupuncture. The other important monographs on moxibustion include Cao Shi Jiu Fang, Gu Zheng Bing Jiu Fang, HuangDi Ming Tang Jiu Jing, etc.
Ancient people always applied direct contact moxibustion to treat diseases. Great developments have been made in modern moxibustion techniques, such as moxibustion with sticks, moxibustion with a moxa burner, warm needle moxibustion and the crude herb moxibustion.
Chapter 5 Acupuncure and Moxibustion Techniques, Clean Needle Techniques
5.1 Acupuncture Techniques with the Filiform Needle (a)
5.1.1 Structure, Specification, Inspection and Storage of Filiform Needles
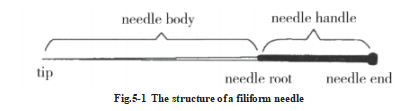
5.1.1.1 Structure
Filiform needles are made of metal. It is best to use stainless steel. They have a straight and smooth shape, great strength and tenacity, formidable resistance to high temperature, rust, and chemicals, and are commonly used in the clinical setting. Other filiform needles made of gold or silver have good heat conductivity, but are seldom used in the clinic practice. Iron and steel needles are used even less clinically, because of their poor flexibility, tenacity, elasticity and their great tendency to rust. The only exception is to occasionally use magnetic needle techniques.
The structure of a filiform needle may be divided into five parts: tail, handle, body, root and tip. (Fig. 5-1) The tipis the sharp point of the needle, also called Zhen Mang, The body is the main part between the tip and the handle. It is named Zhen Ti in Chinese. The root is the part connecting the body and the handle. The handle, the end of the needle from the root to the tail, is the part which the practitioner holds and manipulates the needle. The tail is the end of the handle.
5.1.1.2 Specification of Filiform Needles
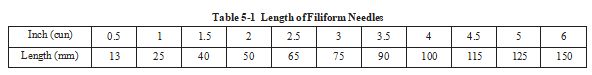
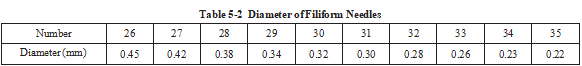
The specifications of filiform needles are distinguished by the diameter and length of the body (see Table5-1, and Table5-2)
5.1.1.3 The Inspection and Storage of Filiform Needles
One should inspect the filiform needles before treatments, especially before primary disinfection. The needle should be disposed of if it is found damaged or otherwise fails to meet the requirements. To prevent the occurrence of accidents in manipulation, the operators must know the methods of inspection, preservation and maintenance.
1. Inspect filiform needles
Pay attention to the following points.
Tip: Traditional needle, the tip should not be too sharp. It is better that the tip be smooth as a pine needle, without hook or curl. But tip of the disposable sterile acupuncture needle is sharp.
Body: The body should be straight, smooth and symmetrical, as well as tenacious and flexible. If the body is curved, rough or rusty, the needle should be disposed of.
Handle: The handle wire should be wrapped around the handle evenly, tightly and continuously. The length of the handle should not be too long or too short. Ensure the needles without corrosion, bending, and nonuniformity of thickness.
Root: The root should be solid and without rust or looseness.
2. Storage and maintenance of traditional filiform needles
The purpose of the storage and maintenance of the traditional needle is to prevent damage to the point of the needle, to protect the needle body from bending, rust, contamination, etc. The general procedure is that the used needles are soaked in the primary disinfection liquid (usually 2% glutaraldehyde solution for more than 40 minutes), rinsed with water after primary disinfection, inserted in a thick gauze pad, with a gauze cover to prevent contamination, then stored in a metal box and put into high-pressure steam sterilization. As the main tool, the filiform needles should be kept and maintained with great care to avoid damage. Otherwise not only will the needles be damaged, but accidents will be more likely in clinical operation. Sterile procedure must betaken seriously. Here are several strategies to consider.
A. If a boiling method is used to sterilize filiform needles, they should be fastened in such a wasy as to avoid causing the tip blunting or curling while touching the disinfection pot in the process of boiling.
B. The filiform needles should be wiped off with a cotton ball or gauze after used. Then put the needles in a needle box or needle tube with a dry cotton ball at both ends to avoid damage to the needle tip. Take care when using the needle.
C. It is best to spread a layer of oil on the needle body, fasten it carefully, and then store it in a hard needle box or needle tube if there is no need for it at the moment.
D. If the filiform needles are placed in a soft clip or pin package, it is better to nip the needles with wood or cardboard to avoid needles’s bending or damage caused by gravity.
3. Maintenance and storage of disposable acupuncture needles
For safety of both practitioners and patients, disposable sterile acupuncture needles have gradually replaced the traditional needles. Disposable acupuncture needles are sterilized by the use of ethylene oxide or gamma rays. Moreover, the package is sealed. The needles should be used within 10 minutes after being taken out of the package. Usuall they can only be used once. Usually packaging is good for 2 years.
Disposable acupuncture needles should be stored in a safe, clean, well ventilated place and avoid suffering from excessive moisture, to control condensation and prevent mold growth.
Sterility may be lost in improper storage conditions before the expiration of validity.
5.1.2 Needling Practice
Manipulation practice is strengthened by practicing. A good manipulation practitioner will be able to swiftly insert a needle through the skin without causing pain or only a slight pain, and will freely manipulate it to produce reinforcing or reducing effects. The patients would like to accept it. The finger force practice and manipulation practice are the foundations for an acupuncture beginner, while skillful techniques are essential for inserting swiftly without causing pain and improving clinical effect. Therefore, it is imperative that a beginner puts forth great effort to develop good finger force and skillful manipulations.
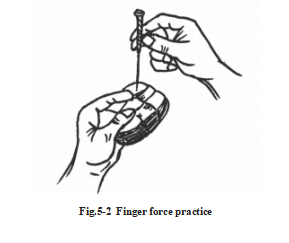
5.1.2.1 Finger Force Practice (Fig. 5-2)
Finger force is the strength generated by the practitioner’s hand when handling a needle. During the process of insertion, strong finger force helps to insert a needle into the body. It is difficult to swiftly insert a needle through the skin and freely manipulate it to lifting and thrusting without reliable finger force, for the body of a filiform needle is very soft. Good finger force is the basis for mastering skillful acupuncture manipulations. Therefore, beginners should practise finger force repeatedly.
At the beginning, to practice with a paper cushion is acceptable. Fold a soft piece of coarse paper or bamboo paper into a small packet of about 7-8 cm ×7-8 cm in size and 2 cm in thickness, and then bind the packet with cotton thread. First to practise it repeatedly with short needles, and then with long needles.
Practice method: Handle the needle like handling a pen, rotate the needle in and out with the thumb, index and middle finger of your needling hand, apply enough pressure for the needle to penetrate the paper and change to another point after that. Repeat this practice until you feel it is easy to do.
5.1.2.2 Manipulation Practice
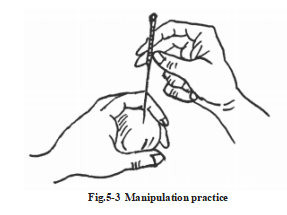
We should not only practice finger force, but also practice manipulation. Skillful manipulation is the basis for acupuncture. Practice twirling and rotating, lifting and thrusting repeatedly and skillfully. Manipulation practice is carried out on the basis of finger force practice. It can be divided into several categories:
1. Quick needling practice
Main points: Press the acupuncture point with thumb and index finger of the lefthand, hold the needle with right hand and insert the tip of needle quickly to a depth of 2-3 mm. Master the speed of insertion by practicing repeatedly so as to reduce pain.
2. Twirling and rotating practice
Main points: The amplitude should be moderate, at uniform angle and speed.
The tip of the disposable acupuncture needles have been changed to dagger shaped and are different from traditional ones whose tips are pine needle shaped. The disposable needles can only bethrusted into the skin, and cannot be twisted into the skin. Thus, you can use twirling manipulation for disposable needles only after it pierces into the dermis.
3. Lifting and thrusting practice
Main points: The extent of movement up and down should be moderate, and the body of the needle should be perpendicular. (Fig. 5-3)
5.1.2.3 Needling Practice on a Body
Practice should be done on yourself or other practitioners after you have developed good finger force and skill in manipulation from practicing on paper packets and cushions. When practicing, try to feel the toughness of the skin, the strength of the pressing fingers and the sensation of the body parts being needled.
5.1.3 Selection of the Filiform Needle
The filiform needle specification depends on sex, age, physique, constitution, nature of disease, interior or exterior location of the disease and location of acupoints. Ling Shu Guan Zhen said that “each of the nine needles, long, short,large or small, has its specific usage.” For example, we use longer and larger filiform needles on male
patients who are muscular or fat, and on patients whose disease is much deeper, and vice versa. The suitable filiform needle length usually equals the depth that the acupoint should be punctured. The needle body should be exposed above the skin a little.
5.1.4 Postural Alignment and Positioning
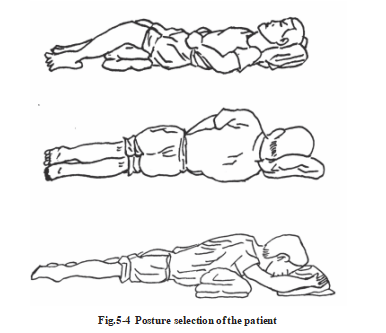
Principle of Postural Alignment and Positioning: In order to make the patients feel comfortable and keep longer during needling, selecting proper position is an important consideration. It is also easy for the operator to select the accurate location of acupoints, needle insertion and manipulation.
The two primary positions most commonly used in the clinic are prone and seated. Such as seated in the upright position with the back leaning against a chair, side-prone sitting, supine position, lateral recumbent, etc. To avoid fatigue or fainting during acupuncture, one should consider selecting the lying position as much as possible for patients receiving their first treatment, or for those who are nervous, old, weak, or seriously ill. (Fig. 5- 4)
5.1.5 Disinfection
5.1.5.1 The Necessity of Disinfection
In the practice of acupuncture, there are four ways in which potential pathogens maybe transmitted: direct contact (between doctors and patients),indirect contact (contaminated equipment and working areas), droplets and air.
It is very important that acupuncturists pay attention to preventing the spread of HIV/AIDS and blood-borne hepatitis viruses, such as Hepatitis B virus and Hepatitis C virus.
Hepatitis B virus can survive for up to 2 weeks on contaminated items.
The latest information shows that Hepatitis C (HCV) on dry surfaces can remain infectious for six weeks.
Besides the patient’s blood, body fluids and excreta, contaminated medical instruments, tools and working areas are also potential sources of infection.
Some inanimate objects, such as the surfaces of magazines, doorknobs, computer keyboards, and waiting room chairs and tables, are often ignored as sources of infection.
Acupuncturists must have a serious attitude towards sterility and practice strict sterile procedure to prevent cross infections andreinfections.
5.1.5.2 Common Ways to Sterilize Needles and Instruments
1. High-pressure steam sterilization
Using 1-1.4 kg/cm2 (pressure) 115-123 ℃for more than 30 minutes. It can be used for the items which cannot be damaged by high temperature, steam or gase, such as glass, rubber and metal products.
You may put a chemical indicator tape inside of an autoclave and judge the result from the changed color. It is the best method of sterilization.
2. Solution soaking sterilization
Glutaraldehyde, which is not corrosive to metal, rubber, glass, or plastic products, is the best disinfectant for instruments. The items to be sterilized are soaked in 2% glutaraldehyde solution for one hour.
(NB: Glutaraldehyde produces a toxic gas, and is irritating to the skin. It must be used in a well-ventilated room. If there is blood on the items, the blood must be removed in advance. The solution should be replaced once a week). The residual disinfectant on the items sterilized must be rinsed off with sterile water and the items must be dried before using.
The items can be soaked in 75% alcohol for 30 to 60 minutes after cleaning and drying, but it is corrosive to plastic products and it is unlikely to be sufficiently effective against hepatitis A virus (HAV). Thermolabile plastic (polyethylene, polystyrene) can be soaked in 1% (10000 mg/L) peracetic acid for 60 minutes. Rinse and clean it with sterile distilled water and dry before use.
3. Sterilization by boiling
Appliances of metal, rubber, glass can be put into the sterilization pot along with boiling water.
Boiled for 30 minutes, the items will be sterile. However, the boiling easily dulls sharp metal instruments.
Adding sodium bicarbonate to the water, to make a 2% solution, can increase the boiling point to 120 ℃. It can also reduce the corrosive effect of the boiling water.
Rubber, glass, etc., can be immersed in detergent or liquid soap and boiled for 30 minutes, and then rinsed, leaned and dried.
Result: Effects of steriliztion are as follows: High pressure >Boil > Drugs.
5.1.5.3 Disinfection of an Acupuncturist’s Fingers and Hands
Wash hands before and after treating each patient if a faucet is available.
Encourage practitioners to wear disposable sterile gloves to protect their own skin and patients.
1. Basic principles for handwashing and hand antisepsis
(1) When the hands have been contaminated with blood or other body fluids, either visible to the naked eyes, or only suspected, practitioners must use liquid soap and running water to wash the hands, and then use alcohol-based hand disinfectant.
If an acupuncturist’s hands have touched blood or other body fluids or secretions from patients, he must wash his hands with liquid soap and running water, no matter how far away the faucet may be. Only by doing so, can he treat the next patient safely.
(2) When the practitioner’s hands have not been contaminated, when there has been no contact with blood, body fluids or secretions, there is no visible pollution, and there are no good handwashing facilities, he should use fast drying hand disinfectant (alcohol-based ) to replace liquid soap and running water for the hands disinfection.
Remember that after contact with blood or body fluids or secretions, practitioners should not just use the alcohol-based hand rub or alcohol-based hand disinfectants for disinfection. Alcohol-based hand disinfectant needs 4 to 10 minutes or more to disinfect HIV in the presence of organic matter (such as blood, body fluids, secretions). A mere 30 seconds of hand scrubbing cannot achieve sterility. Practitioners should wash hands with liquid soap and running water at once.
2. Basic requirements for hand disinfection or antisepsis for practitioners Wash hands before and after puncturing each patient:
(1) If there are good handwashing facilities, use liquid soap to follow the six-step hand-washing method, and wash hands with running water.
Hands should be washed no fewer than two times (15 seconds each time). Then use the fast drying alcohol- based hand disinfectant.
(2) If you do not have good handwashing facilities, or have not touched any blood, body fluids, tissue fluids, or any secretions, then alcohol-based hand disinfectant can be used.
(3) If the acupuncturist’s hands have touched blood or tissue fluids or secretions, he must wash hands three times (each time for 15 seconds) using liquid soap and running water by following the six-step hand-washing method, then dry the hands carefully using a clean paper towel, the and use the alcohol-based hand disinfectant to rub hands for 30 seconds. Then you may handle needles for the next patient.
3. Cautions for finger disinfection
(1) Practitioners should use clean paper towels or tissues to wrap their fingers or use their elbows to turn on or off the faucet to avoid contaminating fingers again. Infrared controlled faucets are a better choice on such an occasion.
(2) Using the elbow to press 2 times can get 3 ml from a hand rub or liquid soap bottle. Pressing with fingers is not allowed.
(3) 3 ml of alcohol-based hand rub or disinfectant must cover both hands for 30 seconds before the operation.
4. Concept of hand hygiene
This refers to the common handwashing technique, the hygienic handwashing technique and the surgical handwashing technique for doctors. They are the most important procedures for controlling infection.
(1) Common hand washing: Refers to the process that most medical personnel use. There is a six-step washing technique using liquid soap and running water to wash hands, remove the dirt, skin flakes and some of the pathogenic bacteria. Each time, washing hands should not last less than 15 seconds. The specific circumstances will determine the times spent for handwashing. One usually washes hands at least twice. If the hands are contaminated by blood, body fluids or secretions, and contamination is visible, hands should be washed at least three times.
(2) Hygiene hand: This refers to the process of hand disinfection when the practitioners use fast dry hand disinfectant or alcohol-based hand disinfectant to rub their hands to reduce the bacteria on the hands.
The total number of bacterial colonies should be no more than 10 cfu/cm2.
(3) Surgical hand: Refers to the process whereby medical staff wash their hands with liquid soap and running water, and then use hand disinfectant to get rid of or kill hand bacteria temporarily on the hand before surgery. The total number of colonies monitored should be less than or equal to 5 cfu/cm2 for surgical hand disinfection.
Acupuncture treatment should at least reach the level of hygienic hand, close to or reaching the surgical hand level.
5. Alternative hand hygiene in special circumstance
If the treatment room is far from a proper sink, does not have good handwashing facilities, and if the hands have no visible contamination and have not touched blood, body fluids or secretions, doctors can use the following process. But if the hands have had contact with blood, body fluids or secretions, and are visibly contaminated, one must immediately wash the hands with liquid soap and running water, the following methods should not be used:
(1) Before or after each performance, practitioners should use qualified hand washing disinfectant or disposable sterilized gel to disinfect their hands. Squeeze liquid 3-5 ml out from the bottle with top of elbow, rub the hands for at least 30 seconds, until the hands dry.
Disadvantages: If the hand scrub is not correctly done, or the disinfection time of hand is less than 30 seconds, there still will be problems. This is the current medical conventional method under circumstances with no blood or body liquid contamination.
For solving these problems, doctors with gloves can add chlorine disinfectants to ensure thorough hand disinfection. For more details, please see the following (2).
(2) Practitioners should wear sterile gloves before performing a procedure:
Before or after each operation, doctors can use sodium dichloroisocyanurate (C3O3N3Cl2Na) or Trichlorinated isocyanuric acid (C3Cl3N3O3) with available chlorine of 1200 mg/L to soak, rubbing hands constantly, for 30 seconds while soaking,then dry hands with paper towels, and finally use an alcohol-based hand disinfectant, to rub on hands for at least 30 seconds.
Due to the fact that the effect of chlorine is greatly influenced by organic matter, chlorine disinfectants need to be changed each time, or whenever the solution becomes turbid.
In the absence of hand disinfectant as in some villages, after washing hands thoroughly 3 times by following six-step methods, each time lasting for 15 seconds, use clean paper towels to wipe and dry the hands. Then use 70%-75% alcohol to rub fingers for at least 30 seconds, before operating the needles.
(NB: Wash hands 3 times instead of twice, because most hand disinfectants not only contain different percentages of ethanol or isopropanol, but also include iodine, chlorhexidinegluconate or triclosan, to enhance the ability to counter hepatitis viruses such as HBV, HCV, etc. )
6. The use of disposable medical sterile gloves Wear gloves under the following conditions:
(1) When there is possible bleeding or emission of other potentially infectious fluids during performance;
(2) Contact with a patient’s membranes, pus discharges, rashes, or broken skin;
(3) The skin on a practitioner’s hand is broken or if a practitioner has HIV or HBV positive;
(4) When using bloodletting therapy in the treatment;
(5) If touching the patient or needling the mouth or genital areas;
(6) If the practitioner suffer from allergies or intolerance e.g, from repeatedly washing hands with liquid soap; sterile disposable gloves are the first layer of protection for the practitioner:
If there are more than 20 patients, the practitioner should use a new pair of sterile gloves for each patient. It is not necessary to wash hands. Just rub both hands using hand disinfectant for 30 seconds, and then start the next operation.
If time permits, there are not many patients, and the practitioner has not touched blood, body fluids, or secretions, he may use the methods described above, such as those mentioned in 3.5.1(2) for hand disinfection. This method can save gloves.
5.1.5.4 Disinfection of Acupuncture Area
Use a cotton ball soaked in a 70% to 75% alcohol solution to wipe the acupuncture area on a patient. Wiping should be in a rotary scrubbing motion, spiraling out from the center.
If dirt is visible, it should be washed off first. After cleaning the skin, avoid contaminating it again and keep it clean. Or use 2% iodine to clean, dry for a while, and then use a 75% alcohol cotton ball to wipe off iodine, or wipe with 0.5%-1.5% iodophor.
5.1.5.5 Sterilization of Treatment Rooms
All the surfaces and facilities in treatment rooms need to be cleaned with diluted detergent regularly and often (medical personnel should wear overalls and gloves). Standard intensity ultraviolet can also be used for irradiation.
Normall, one can use chlorine disinfectant or bleach solution (such as sodium hypochlorite 1:100 or household bleach).
A 500 mg/L chlorine solution, a 3% hydrogen peroxide, phenolic compounds, or chlorhexidine may also be used for routine cleaning.
Disinfection for sterilizing work clothes:
Use solution containing chlorine of 1200 mg/L to soak the dirty work clothes for 30 minutes, or soak in a 6000 mg/L chlorine solution for 10 minutes,and then wash with common liquid soap.
Obvious bloodstains on work clothes need to be soaked in 1:10 solution of household bleach or detergent containing 6000 mg/L available chlorine for 1-2 hours, and then cleaned again with 90 ℃ water, or boiling or high pressure sterilization can be also used. Work clothing contaminated with a large amount of blood can be disposed as medical waste.
5.1.5.6 Processing of Occupational Exposure
Because of the risk of occupational exposure, acupuncturists have to be vaccinated against hepatitis B. Here are a few suggestions and measures:
(1) If an acupuncturist is accidentally stabbed, he should act quickly. Let the injury bleed. If a finger is injured but there is no obvious bleeding, let the finger hang down until blood flows out. Perhaps he should or squeeze the wounded area to make it bleed.
Meanwhile, wash the wound with a large amount of water for more than 10 minutes. Use skin disinfectant to clean the area around the wound and then wrap the wound with sterile gauze.
(2) Assessing the patient’s condition
The practitioner should examine the patient’s medical records and question the patient in order to assess risks. If the patient does not know or make sure that he/she has the hepatitis B virus (HBV), hepatitis C virus (HCV), or human immunodeficiency virus (HIV), the practitioner should urge them to have an examination for blood-borne pathogens (or send the patient's blood for test under patient’s consent). Afterwards, the agreement should be added to the patient’s medical records.
(3) Workers should be sent to the Infectious Diseases Department or Emergency Department for further evaluation, so that preventive measures or treatment can betaken as soon as possible, for example blocking HIV or HCV preventive medication.
(4) Recording the accident, protective measures for accidents and names or states of blood-borne pathogens. According to the requirements of local Provincial Health Regulators, the practitioner should submit a timely report to the proper agency.
5.1.5.7 How to Deal with Waste Such as Used Needles
Waste can be roughly divided into general wastes and biological medical wastes.
The biological medical wastes are the solid, liquid and sharp instruments containing potential infection risk from biological sources.
They must be disposed of carefully to prevent infection to others.
The common medical wastes from acupuncture are sharp instruments (acupuncture needles, dermal needles, triangular needles, intradermal needles, and any other things likely to pierce the skin). They may include other things contaminated with blood and body fluids, such as cotton swabs.
Anyone using sharp instruments has the responsibility to ensure the safe disposal of acupuncture needles and other sharp instruments. Used sharp instruments must be thrown into a hard box. The box should be unbreakable, and without leaks under normal conditions.
For safe carrying, it is recommended that the practitioner use a box with a handle and a lid. There ought to be a label on the box with biological hazard warning signs. It must be kept in a place where children cannot reach.
When discarding needles, hands should not touch the box holding sharp instruments, to avoid contamination. Sharp instrument boxes should be changed when two-thirds to three-fourths full.
The biological medical wastes which are not sharp instruments should be thrown into a special bag colored yellow or red, and labeled. They should be disposed of according to local regulations.
When removing biomedical wastes, you must deliver them to companies which are licensed for the safe disposal of medical wastes.
5.1.5.8 Sanitary Facilities Required for Hand Washing and Hand Disinfection
(1) Diagnosis and treatment areas should have plumbing facilities for washing hands. The faucets should be able to be turned on without hands touching them.
(2) Clinics should be equipped with hand antiseptics: liquid soap, and proper alcohol-based hand disinfectant or fast hand disinfectant. (They should have a license or code from the Ministry of Health. The practioner must pay attention to the period of validity.)
(3) Clinics should be equipped with proper hand drying materials, such as clean and dry paper towels, or other facilities, in order to avoid secondary contamination.
(4) Rubbish bins should be stationed near the sinks for easy operation.
5.1.5.9 Mandatory Requirements for Using Running Water to Wash Hands
Under the following circumstances, practitioners must immediately use soap (liquid soap) and running water to wash their hands, and then use alcohol-based hand disinfectant for sterilization.
(1) When the hands have or are suspected to have touched blood or other body fluids;
(2) When the hands are visibly contaminated;
(3) When the hands have touched materials contaminated by infectious pathogenic microorganisms;
(4) When the hands have touched patients with infectious diseases or after processing contagious pollutants.
Supplement:
Updated Research of Clean Needle Technique
1. Study on the relationship between the number of times hands are washed and how long they are washed each time, and the effects these variables have on sterilized hands.
Sheng[1] observed the effect of the medical staff using the general hand washing technique after 1 to 3 times ’ washing. He divided them into 5 groups. Some washed for 5 seconds each time, some for 10 seconds each time, some for 15 seconds, some for 20 seconds, and others for 25 seconds. For the groups who washed for 10 seconds, 2 times, bacteria decreased from 436 cfu/cm2 to 52 cfu/cm2; 3 times, to 4 cfu/cm2. For the 15 seconds group, washed hands after 1 time, germiculture dropped from cfu/cm2 1000 to 216 cfu/cm2, 2 times to 8 cfu/cm2, 3 times to 4 cfu/cm2 group of 20 secnds, washed hands 1 time, bacteria culture from 348 cfu/cm2 down to 9 cfu/cm2.
Conclusion: Each time the practitioner should scrub hands for at least 10 seconds for 3 times, to meet hospital infection control standards (skin flora ≤10 cfu/cm2).
The longer one washes his hands with soap, the fewer bacteria there will be. Therefore, when wash your hands, the process of careful scrubbing for a longer period cannot be ignored.
2. Modern research on the effects of commonly-used disinfectants and antiseptics on killing HIV, HBV and HCV micro-organisms among acupuncturists.
(1) Ethyl alcohol: The effective concentration of alcohol generally ranges from 60% to 90% [2]. According to the report[3], 70% ethanol takes 2 minutes to kill drying HIV, but inactivated dried serum HIV requires 4 minutes. If the materials contain proteins, even longer time is needed. Because alcohol is quite volatile, it is necessary to soak the object for 10 minutes for inactivation. Some reports indicate that 75% alcohol can kill the HIV virus, in suspended liquid, only within 30 seconds[4] . Other reports say that 70% ethanol cannot inactivate HIV within 10 minutes[5] . 70%-75% alcohol has no effect on hepatitis A virus (HAV), and its effect on hepatitis B virus remains controversial (the virus is not completely inactivated) [2] .
1 - propanol more than 30% and 2-propanoland ethanol above 60% concentration can kill HCV on drying objects within 1 minute[6]. 70% isopropyl alcohol can kill HCV, HBV and HIV in 10 minutes, while it can clear HIV-1 on drying objects within 1 minute and destroy infectivity[2] .
(2) Chlorine disinfectant: sodium dichloroisocyanurate (C3O3N3Cl2Na) and trichlorinated isocyanuric acid (C3Cl3N3O3) are the most commonly used chlorine disinfectants. In the presence of 8% serum, 100 ppm available chlorine in the disinfectant test mixture inactivated 3.75 log TCID50 HIV/ml within 30 seconds. In the presence of 80% blood, 1,000 ppm available chlorine in the disinfectant test mixture was unable to inactivate[7] . In the presence of 100% blood, 5,000 ppm available chlorine in the disinfectant test mixture was unable to inactivate HIV in 20 minutes[4] .
In cases where prior cleaning is impossible, in the presence of high levels of organic matter, care must be taken to use the higher recommended concentration (aminimum of 10,000 ppm available chlorine)[7] . Since it is greatly influenced by organic matter, available chlorine concentrations in chlorine disinfectants should inactivate HBV between 500 mg - 100 g/L use[8] . WHO suggests that those processing contaminants use 5,000 mg/L chlorine disinfectants for at least 10 minutes, while the US Center for Disease Control recommends those handling blood use 5,000 mg/L chlorine disinfectants to inactivate all blood-borne viruses, including spores[9] .
The British standard recommends processing general contamination with a concentration of available chlorine 1,000 mg/L. Serious contamination should be treated with 10,000 mg/L chlorine disinfection disinfectant[7] .To inactivate hepatitis C virus (HCV), one needs an antiseptic containing an available chlorine content of 1,200 mg for half an hour-6,000 mg/L for more than 10 minutes. But the effective chlorine 900 mg/L or below cannot inactivate HCV-DNA[10][11] .
(3) Glutaraldehyde: 0.1% glutaraldehyde in plasma contaminated with HIV takes effect in 5 minutes, while 0.05% glutaraldehyde will also sterilize HIV viruses suspended in liquid in 5 minutes[4] . A 2% glutaraldehyde solution needs 1-2 minutes to inactivate HIV, HAVrequires 1-10 minutes, while HbsAg, needs 30 minutes[12][13][14], and anti-HCV, 5-20 minutes [14] .
(4) Peroxyacetic acid: the effective component of 5 g/L or 0.5% peroxyacetic acid, C2H4O3, has no sterilizing effect on the HIV virus in whole blood or plasma within 20 minutes. For the HIV in the suspension, the effective component of 100 mg/L peracetic acid can have an effect within 3 minutes. For a 1% peracetic acid to inactivate HBsAg it needs 30 minutes. 1% peracetic acid takes 60 minutes to inactivate HBV DNA. 0.5% peracetic acid needs 60 minutes to inactivate HBsAg, while 0.5% peracetic acid can not inactivate HBV-DNA within 60 minutes[15] .
(5) Iodophor: 0.5% iodophor destroying HBsAg and HBV-DNA needs 2-60 minutes[12][16] HAV 1-10 minutes, anti HCV 5-30 minutes[13] [14] [18], 0.2% iodophor inactivating HBV-DNA 10 minutes[16] .
(6) Hand disinfectant or hand antiseptic: Ciesek[19] reports that hand disinfectant containing different percentage of ethanol or isopropanol, including iodine, Chlorhexidine Gluconate or triclosan can inactivate 6 logarithm of HCV in a liquid suspension within 30 seconds when undiluted. But hand disinfectant composed solely of alcohol loses its inactivating effect for HCV after diluted.
3. Basic principles of Clean Needle Technique (CNT): (from Clean Needle Technique Manual for Acupuncturists, Sixth Edition Published by The National Acupuncture Foundation 2009, USA).
Clean needle technique (CNT) includes the following basic principles:
(1) Always wash hands in the intervals between treating patients, both before and after needling.
(2) Always wash hands immediately after contact with potentially infections body fluids such as blood, body fluid, secretion of patient, or obvious environmental contaminants.
(3) Always use sterile single-use needles and other instruments that may break the skin, such as seven- star hammers and lancets.
(4) Always establish a clean area before performing acupuncture.
(5) Always immediately isolate used needles and other sharp instruments.
References
[1] Sheng LL, Zhu YQ, Wang GL. The research about the soap washing time and related effect [J]. The Chinese Journal of Hospital Infection, 2002, 12(7):508.
[2] Yin Y, Zhang LW. Development of alcohol disinfectants and their preparations [J]. Chinese Journal of Disinfection, 2013, 30(11): 1062-1063.
[3] Van Bueren J, Cooke EM, Mortimer PP, et al. Inactivation of HIV on surfaces by alcohol [J]. BMJ, 1989, 299(6696): 459.
[4] Chen LY,Wu SL, Lin LW, etc. Evaluation of disinfection efficacy on HIV with different disinfectants [J]. Chinese Journal of Public Health, 2013, 29(8): 1111-1114.
[5] Hansen PJ. Chemical inactivation of HIV on surfaces [J]. BMJ, 1989, 299(6693): 260.
[6] Doerrbecker J, Friesland M, Ciesek S. Inactivation and survival of hepatitis C virus on inanimate surface [J]. Infect Dis, 2011, 204(12): 1830-1838.
[7] Van Bueren J, Simpson RA, Salman H, etal. Inactivation of HIV-1 by chemical disinfectants: sodium hypochlorite [J]. Epidemiol Infect, 1995, 115 (3): 567-579.
[8] Li XJ, Liu JH. Nosocomial infection and disinfection of blood transmitted hepatitis [J]. Chinese Journal of Blood Transfusion, 1999, 12(3): 205.
[9] http://www. cdc. gov/hicpac/Disinfection_Sterilization/5_0cleaning.html Guideline for Disinfection and Sterilization in Healthcare Facilities, 2008.
[10] Xuan DP. Evaluation of the efficacy of sodium hypochlorite in the treatment of hepatitis C virus [J]. Transportation medicine, 1999, 13(1): 89.
[11] Li XJ. Study on disinfection of HCV positive serum contamination by several commonly used disinfection methods [J]. Practical
Preventive Medicine, 2000, 7(4): 311.
[12] Cheng B, Wei B. Evaluation to inactivation of HBsAg of disinfectants [J]. International Journal of Laboratory Medicine, 2014, 35(12): 1651-1652.
[13] Zhang EN. Comparison of the inactivation effect of commonly used disinfectants on HAVHBsAg and HCV [J]. Journal of Practical Traditional Chinese Medicine, 2003, 19(3): 109.
[14] Zhang LG, Ma F, Zhang LC. The evaluation about inactivation effect of commonly used disinfectant to HAV, HBsAg and anti - HCV effect on oral instruments [J]. Journal of Practical Nursing, 1997, 13(11): 598.
[15] Yang Y, Gong YW. Disinfection effect of peracetic acid on HBV contaminated needles [J]. Journal of Practical Medicine, 2003, 20(3):203.
[16] Lian P, Su X. Experimental study on inactivation effect on HBsAg and HBV - DNA by iodophor solution [J]. Journal of Jining Medical College, 2002, 25(3): 45.
[17] Kobayashi H, Tsuzuki M, Koshimiza K, et al. Susceptibility of hepatitis B virus to disinfectants or heat [J]. Clinic Microbiol, 1984,20(2): 214-216.
[18] Wang X. Experimental report on inactivation of hepatitis C virus RNA by commonly used disinfectants [J]. Anhui Journal of Preventive Medicine, 1999, 5(2):171.
[19] Ciesek S, Friesl and M, Steinmann J, et al. How stable is the hepatitis C virus (HCV) enviromental stability of HCV and its susceptibility to chemical biocides [J]. Infect. Dis. 2010, 201(12):1859-1866.
5.1.6 Acupuncture Techniques
5.1.6.1 Insertion
It is refers to an operation method of inserting a needle into the skin.
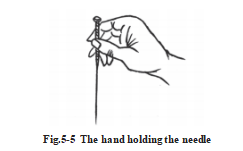
The right hand holding the needle is generally known as the “puncturing (needling) hand” . The puncturing (needling) hand holds the handle of a needle with the thumb, the index finger and the middle finger, and the thumb finger palp is opposite to the index finger and the middle finger, like handling a chinese writing brush. (Fig. 5-5)
The other hand assisting or pressing the body part is the “pressing (palpating) hand” .
The function of the puncturing hand is to hold the needle and operate manipulations. During insertions, the puncturing hand generates focused force on the tip of the needle to make it penetrate the skin. During manipulation, it twirls and rotates, lifts and thrusts, plucks and vibrates and withdraws the needle.
The function of the pressing hand is to fix the location of a point and to grip the needle body to help the puncturing hand insert the needle. It can support the body of the needle, keep it straight and focus the pressure directly on the tip of the needle, resulting in a good insertion and less pain, while facilitating the control of the needling sensations.
Nan Jing said: “Those who know a lot about acupuncture believe in their left hands, while the ones who do not, believe only in their right hands.”There are various ways of doing an insertion:
1. Single-Handed Insertion: The practitioner just uses one hand for needle insertion. It is used for short needles.
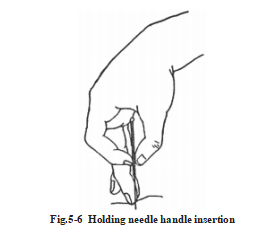
(1) Holding needle-handle insertion: Holding the needle with the right thumb and index finger, the tip of the middle finger touches the skin close to the acupuncture point, the pad or distal part of the middle finger supports the body of the needle. When the thumb and the index finger push downwards, the middle finger will also be buckling, the acupuncture needle will be inserted to the required depth. (Fig. 5-6)
(2) Holding needle-body insertion: Use the pad of the thumb and the index finger or the thumb and the middle finger of the right hand to clamp the lower end of the needle body, so that the tip of the needle is stretched out to the length of 2/10~3/10 needle Cun (approximate 1.5 mm or 2 mm). Pointing to the location of the acupuncture point, the needle is inserted vertically into the acupuncture point, and then twist the needle inside to a certain depth.
2. Double-Handed Insertion: It involves the use of both hands working in concert with each other.
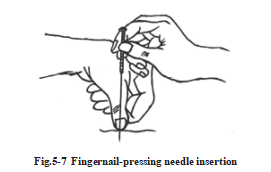
(1) Fingernail-pressing needle insertion: Press the acupuncture point with the thumbnail, or the index finger of the lefthand/pressing hand. Hold the needle with the right hand/puncturing hand and keep the needle tip closely against the border of the nail of the pressing hand. This method is suitable for puncturing with short needles. (Fig. 5-7)
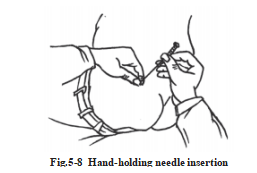
(2) Hand-holding needle insertion: Hold a dry, sterile cotton ball around the needle tip with the thumb and the index finger of the pressing hand/lefthand and fix the needle tip directly over the selected point. Hold the handle of the needle with the puncturing hand/right hand and both hands insert the needle into the point simultaneously. This method is suitable for puncturing with long needles. (Fig. 5-8)
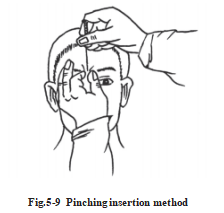
(3) Pinching insertion method: Pinch the skin up around the point with the thumb and index fingers of the pressing hand/lefthand. Hold the needle with the puncturing hand/right hand and insert the needle into the point in the pinched skin. This method is suitable for puncturing acupoints on areas where the muscle and skin is thin, such as Yintang (EX-HN 3). (Fig. 5-9)
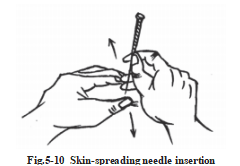
(4) Skin-spreading needle insertion: Put the thumb and index fingers of the press hand/lefthand on the skin where the point is located and separate the two fingers to stretch the skin taut. Hold the needle with the puncturing hand/right hand and insert the needle into the point through the space between the two fingers. This method is suitable for needling acupoints on areas where the skin is loose. (Fig. 5-10)
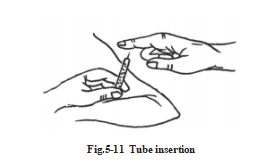
3. Needle in Tube Insertion: Put the needle into a stainless steel, glass or plastic tube instead of doing pressing hand insertion. (Fig. 5-11)
5.1.6.2 Direction Angle, and Depth of Insertion
During the process of insertion, the angle, the direction and the depth are especially important. Correct direction angle, and depth help to increase needling sensations, bring about the desired therapeutic effects and guarantee safety. Clinically, using different directions angles, or depths of insertions, even on the same points, will lead to needling sensations that have obviously different transmission directions intensities, and therapeutic effects. The directions, angles and depths of insertions are decided according to the specific location of the acupoint, the physical condition the of a patient and the nature of an illness.
1. Direction of Insertion: The direction of insertion refers to the direction of the needle tip during acupuncture. Generally, it depends on the direction of the meridians, the location of a point and the desired therapeutic requirements of an illness.
a. In accordance with the meridian flow: By virtue of the direction of the needle tip, needling a point by going in the direction of the normal flow of the course of its meridian, or against its meridian course, will yield reinforcing or reducing effects.
b. In accordance with the location of the acupoint: Deciding the direction of insertion according to the location of the acupoint ensures the safety when needling. For instance, the needle should be inserted slowly, with the tip pointing in the direction of the mandible when puncturing Yamen (GV 15), and however, towards the root of tongue when puncturing Lianquan (CV 23).
c. According to the therapeutic requirements of a disease: “To promote the movement of the meridian qi to reach the diseased area”, the needle tipis pointed to the area of disease.
For instance,tennis elbow, acute posterior ganglionitis. Yintang (GV 29) is for the treatment of rhinitis or headache.
2. Angle of Insertion: The angle of insertion refers to the one formed by the needle and the surface of the skin as the needle is inserted. It is decided in consideration of both the location of the point and the doctor’s purpose. Generally, there are three options: perpendicular insertion, oblique insertion and horizontal insertion. (Fig. 5-12)
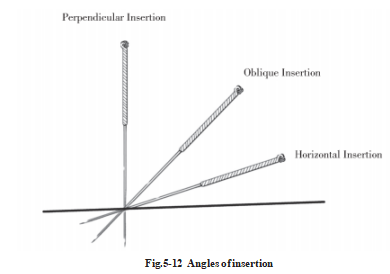
a. Perpendicular Insertion: The needle is inserted perpendicularly, forming a 90° angle with the surface of the skin. Most points on the body can be needled in this way. Both deep insertions and shallow insertion are advisable, especially for the acupoints in the muscular areas, such as limbs, abdomen, and waist.
b. Oblique Insertion: The needle is inserted obliquely to form an angle of approximately 45° with the skin’s surface. This is suitable for acupoints which are applicable to the edge of the bone, where internal organs are close to the surface of the body, or where there are bloodvessels and scars, such as the acupoints of chest and back.
c. Horizontal Insertion: It is also known as transverse or subcutaneous insertion. The needle is inserted horizontally to form a 15° . This method is suitable for points where there are few underlying tissues, such as the acupoints of head.
3. Depth of Insertion: Depth of Insertion refers to how deep the needle body is pushed into skin. Generally, each acupoint has its definitive needling depth (See Acupoints). We will introduce the following situations.
a. Constitution of the Patient: Relatively shallow insertions should be done on lean weak patients, and deep insertions on strong, robust patients.
b. Age: As elderly patients and infants have delicate constitution, deep insertion is inadvisable where it is concerned. However, young and middle-aged patients are usually able-bodied; therefore, appropriate deep insertion may be practiced on them.
c. Pathological Condition: Yang syndromes and acute diseases should be treated with shallow insertion; while yin syndromes and chronic illnesses with deep insertion.
d. Location of the Points: Points on the head and face, chest and back, and areas where the skin and muscles are thin should be punctured superficially. Deep insertion is appropriate for points on the four extremities, the abdomen and thick, bulky areas.
The angle of insertion relates closely to the depth of insertion. Generally speaking, deep insertions often go with perpendicular insertions, while shallow insertions go hand in hand with oblique or horizontal insertions. The angle and depth of insertion must be well mastered when needling points such as Tiantu (CV 20), Yamen (GV 15),Fengfu (GV 16), and points on the areas around the eyes, on the back and close to internal organs, such as heart, liver and lungs.
5.1 Acupuncture Techniques of the Filiform Needle (b)
5.1.7 Manipulations and the Arrival of Qi
Manipulations, also known as needling transmissions, are done following insertions designed to produce needling sensations, regulate the intensity of needling sensations, or to reinforce and reduce. The arrival of qi, also termed a “needling sensation”, refers to the responses produced in the meridian qi after a needle has been inserted into an acupoint to certain depth and then manipulated. Generally, manipulation techniques can be divided into two categories, fundamental and auxiliary.
5.1.7.1 Fundamental Manipulation Techniques
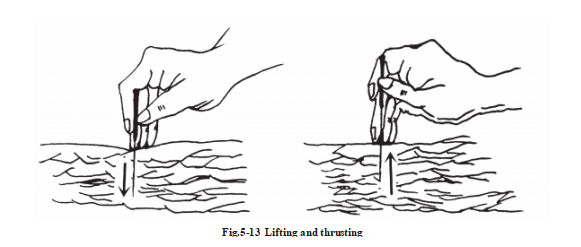
1. Lifting and Thrusting: This is a method whereby the needle body is lifted and thrust perpendicularly into the point after the needle has been inserted to a certain depth. Thrusting involves inserting the needle from the superficial layer down to the deeplayer. By contrast, lifting involves withdrawal of the needle from the deeplayer up to the superficial layer. (Fig. 5-13)
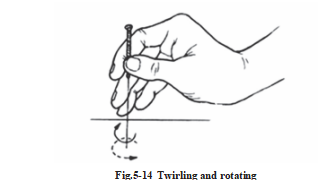
2. Twirling and Rotating: This is a method that involves twirling or rotating the needle handle continuously, backwards and forwards, by holding with the thumb, the index finger and the middle finger of the right hand after it has reached the desired depth. (Fig. 5-14)
These two basic techniques can be used separately or in conjunction with each other.
5.1.7.2 Auxiliary Techniques
The auxiliary techniques are supplements to the fundamental ones. The ones that are commonly used in the clinical setting are as follows:
1. Massaging along the meridian: After inserting the needle into the acupoint to a certain depth, gently press or tap the skin along the course of the meridian where the acupoint is located at or around the acupoint with the finger-pads moving upward and downward, or left and right. (Fig. 5-15)
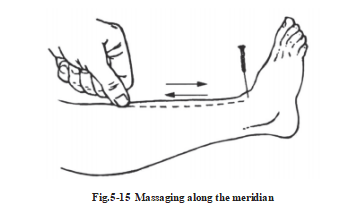
This method may induce the circulation of the channel qi, to make qi and blood regular and circulated. If the doctor feels heavy and tight sensations in the fingers, pressing will accelerate the movement of the qi and blood.
2. Scraping: After the needle has been inserted to a specific depth, support the tail of the needle with the pads of the index finger and the thumb while scraping the handle of the needle frequently from top to bottom or from bottom to top, with the nail of the thumb, the index finger or the middle finger. (Fig. 5-16)
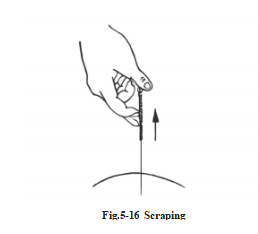
If the needling sensation does not arrive, it can be stimulated using this technique. If the needling sensation has already arrived, it will transmit and diffuse the sensation with more intensity.
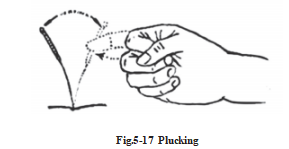
3. Plucking: This technique involves plucking the needle’s tail or handle slightly with the fingers, causing it to gently vibrate. It should not be plucked too hard and too fast to avoid bending. Plucking has the function of stimulating and invigorating the qi. (Fig. 5-17)
4. Twisting: After the needle has been inserted to a specific depth, twist and rotate the needle’s handle uniaxially inward or outward with the thumb, the index finger and the middle finger of the right hand, like rolling lines (2-3 circles or 3-5 circles each time. It should be used in conjunction with the lifting and thrusting method, so as to avoid the needle body intertwining with the muscle fiber). (Fig. 5-18)
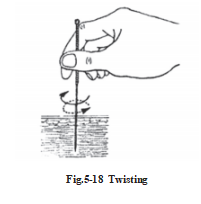
If the needling sensation does not arrive, it can be stimulated by using this technique; if the needling sensation has already arrived, it will enhance the sensation.
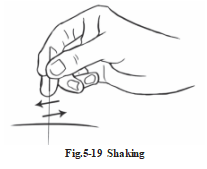
5. Shaking: After the needle has been inserted to a specific depth, hold the handle and shake it gently, like wielding a boat’s oar or turning a windlass. It will intensify the needling sensation. (Fig. 5-19)
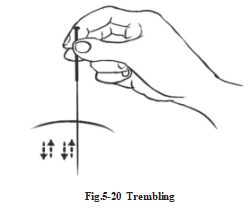
6. Trembling: After the needle has been inserted to a certain depth, hold the needle with fingers of the right hand and apply quick lifting and thrusting, or twirling and rotating movements in small amplitudes to create gentle vibrations. This promotes the arrival of qi. (Fig. 5-20)
5.1.7.3 The Arrival of Qi, Waiting for Qi, Promoting Qi and Maintaining Qi
1. The arrival of qi: The arrival of qi was first mentioned in Nei Jing. It refers to the responses produced in the meridian qi after a needle has been inserted into an acupoint to a certain depth and then manipulated with lifting and thrusting, twirling and rotating. It is also known as “needling sensation” .
When the qi arrives, the practitioner may feel a demulcent or tensional sensation around the needle. The patient may also have sensations of soreness, distension, numbness, or heaviness. Sometimes he may feel the sensation radiating in a specific direction or to a specific place. If the qi does not arrive, the patient will have no corresponding feeling or reaction, and the practitioner might feel an emptiness, or loose, slippery sensation around the needle. Dou Han-qing said in Biao You Fu: if you feel a loose, slow, slippery sensation around the needle, qi has not arrived; if you feel a tensional, dragging sensation around the needle, qi does arrive……when qi a rrives, you feel like a fish has swallowed your bait, or else you just feel as still as standing by a lake.
Whether the qi arrives or not, and the speed at which it arrives, directly influences the therapeutic effect of acupuncture. It is also the basis for determining the patient’s prognosis. Ling Shu·Jiu Zhen Shi’er Yuan says: “If qi has not arrived, doctors must wait till it has arrived, and should not worry about the time. When qi has arrived, it must be withdrawn … . ” The key to acupuncture’s therapeutic effect is the arrival of the qi. It emphasizes the significance of the arrival of the qi. Usually the faster the qi arrives, the better the therapeutic effect will be. If qi does not arrive, it is possible that there will be no beneficial effect. Jin Zhen Fu (The Golden Needle Ode) also says: “The rapid arrival of qi suggests good effects during a treatment; the slow arrival of qi is an indication of retarded effects in a treatment.”
Therefore, if the qi does not arrive in your clinical practice, you must analyze and discover the reasons: an inaccurate acupoint location, an improper needle manipulation, an incorrect angle and/or a needling depth may be at the root of the problem. Once any of these problems has been rectified, the qi will usually be obtained. It is difficult for the qi to arrive when weak patients are being treated or those in a pathological condition. We can promote the arrival of qi, wait for the arrival of qi by allowing the needle to stay in the acupoint, or using a warm- needle moxibustion, a moxa stick. These methods can promote the arrival of qi. If qi has not arrived after using the former methods, it is because the qi ofzang, fu and meridians have become extremely weak. In this situation, we should consider using other methods.
2. Waiting for the arrival of qi: Waiting for the arrival of qi means that when qi does not arrive, one should allow the needle to stay in the acupoint for a longer time; you can also manipulate it at intervals to wait for the arrival of qi. Zhen Jiu Da Cheng says: Waiting for qi arrivals is a priority in all techniques of acupuncture.
3. Promoting the arrival of qi: One can accelerate the arrival of qi by using various types of manipulation, such as lifting and thrusting, twirling and rotating, shaking, massaging and scarping, or twirling the needle handle slightly.
Promoting the arrival of qi is a method of stimulating the arrival of qi.
4. Maintaining the needling sensation: It is the key to the clinical curative effect. Once the qi has been obtained, one should maintain the qi carefully and not lose it.
5.1.8 The Reinforcing (Tonification) and Reducing (Dispersal) Methods of Acupuncure
Ling Shu ·Jing Mai points out that: “ Deficiency syndromes should be reinforced, excessive syndromes should be reduced,heat syndromes should be swift, cold syndromes should be retained, while depression syndromes should be treated with moxibustion.” This establishes the principle of tonifying deficiencies and reducing excesses when performing acupuncture manipulation. Therefore, reinforcing and reducing in acupuncture is of great importance in treating diseases with acupuncture and is one of the essential parts of acupuncture techniques.
The Reinforcing Method of Acupuncture: It refers to the method of strengthening the right qi (zheng qi) and restoring the normal functions of the viscera from a subdued state.
The Reducing Method of Acupuncture: It refers to the method of expelling pathogens, reducing the excess, and restoring the normal functions of the viscera from an excited state.
The reinforcing and reducing methods of acupuncture are intended to stimulate acupoint, while adopting
feasible manipulations in order to restore the normal functions of the viscera, supplement the right qi (zheng qi) by regulating the meridian qi that helps strengthening the weakened physiological function and regulating the functions of viscera organs and meridians, so as to restore health by maintaining balance of yin and yang.
5.1.8.1 Single Method
1. Basic Reinforcing and Reducing Methods
a. Twirling and Rotating (Nian zhuan): After the needle has been inserted to a given depth and the qi has arrived, rotate the needle slowly and gently with small amplitudes for a relatively short period of time. This is called reinforcing.
Conversely, reduction is done by rotating the needle strongly and rapidly with large amplitudes for a relatively long period of time.
When using the reinforcing method, move the thumb forward, move the index finger backward, and turn left mainly.
When using the reducing method, move the thumb backward, move the index finger forward, and turn right mainly.
b. Lifting and Thrusting (Ti cha): Following the insertion of a needle to a given depth and after obtaining the needling sensation, reinforcing is achieved by lifting the needle rapidly and forcefully, while thrusting the needle slowly and gently with slow amplitudes for a relatively short period of time. Conversely, reduction is done by lifting the needle slowly and gently, while thrusting the needle rapidly and forcefully with fast amplitudes for a relatively long period of time.
2. Other Reinforcing and Reducing Methods
a. Rapid and Slow Insertions and Withdrawals (Xuji):
Reinforcing Method: Insert the needle into the deeplayer slowly and withdraw it rapidly after inserting it into the dermis.
Reducing Method: Insert the needle into the deeplayer rapidly and withdraw it slowly after inserting it into the dermis.
b. Directing the Needle Tip (Ying sui):
Reinforcing Method: Point the tip of the needle, during an insertion, in the same direction of the normal flow or course of the meridian pathway.
Reducing Method: The needle tipis pointing in the opposite direction, going against the normal course of the meridian pathway.
c. Breathing/Respiration (Hu xi):
Reinforcing Method: Insert the needle when the patient breathes in and withdraw the needle when the patient breathes out.
Reducing Method: Insert the needle when the patient breathes out and withdraw the needle when the patient breathes in.
d. Open-Close Method (Kai he):
Reinforcing Method: Cover and press the needle hole to quickly close it when withdraw the needle.
Reducing Method: Shake the needle to enlarge the hole prior to withdrawing it, and do not cover and press the hole.
e. Even Method (Ping bu ping xie): When the needle is inserted into the point and the needle sensation is achieved, lift, thrust and rotate the needle evenly. This method is suitable for treating inconspicuously deficient or excessive syndromes, or syndromes with both deficiency and excess.
5.1.8.2 Comprehensive Reinforcing and Reducing Methods
Comprehensive reinforcing and reducing method is the comprehensive application of the single methods. It is a method that combines various other methods by which the operation is completely different but the effect is the same, for the purpose of reinforcing and reducing.
1. Setting the Mountain On Fire (Shao shan huo): This method is suitable for treating paralysis and numbness due to cold syndromes and yang deficiency.
Operating points: reinforcing method of twirling and rotating + reinforcing method of breathing.
Upper (heaven)→middle (human) →lower (earth): After the needle has been inserted, push it to each portion and employ the reinforcing method by twirling and rotating 9 times after the qi arrives. Repeat the above- mentioned proces several times and back the needle to the lower (earth) portion and retain it there.
This process can be done in conjunction with reinforcing by means of respiration.
2. Penetrating - heaven’s coolness (Tou tian liang): This method is suitable for treating excessive heat syndromes like paralysis and acute carbuncles.
Operating points: Reducing method of twirling and rotating + reducing method of breathing.
Lower (earth)→middle (human) →upper (heaven): After the needle has been inserted to lower portion, lift it to each portion and employ the reducing method by twirling and rotating 6 times after the qi arrives. Repeat the above-mentioned process several times and retain it at upper (heaven) portion. This process can be done in conjunction with reducing by means of respiration.
5.1.8.3 Factors that Can Influence the Therapeutic Effects of Reinforcing and Reducing
The effect of reinforcing and reducing is mainly determined by the following three aspects:
1. Physical and Mental Status: One can regulate the different therapeutic effects of acupuncture by using the reinforcing or reducing method according to the patient’s medical condition. When the body is weak and deficient, acupuncture can strengthen the right qi (zheng qi); on the other hand, when there are exuberant pathogens, such as excessive heat, acupuncture can clear the heat, dredge the obstruction, expel pathogens and reduce the excess.
In the case of cramps due to gastrointestinal hyperactivity, acupuncture can alleviate the cramps and pains by reinforcing the function of the digestive tract. If the peristaltic action of the patient’s intestines is retarded, acupuncture can promote peristalsis and digestive function, eliminate abdominal distension, and increase the appetite.
2. The Relative Specificity of Acupoints: The indications of acupoints not only have universality, but also relative specificity. Some acupoints, such as Zusanli (ST 36) and Guanyuan (CV 4), can invigorate the right qi (zheng qi) and strengthen the body. Some other acupoints, such as Shixuan (EX-UE 11),Shaoshang (LU 11) dispel pathogens, and restrain hyperactive functioning in the body.
3. Needles and the Force of Manipulation: It is an important part of the realization of the reinforcing and reducing by promoting the transformation of human intrinsic factors.
5.1.9 Retention and Withdrawal of Needles
5.1.9.1 Needle Retention
Needle retention means to retain the needle in the acupoint after it has been inserted. Su Wen·Li He Zhen Xie Lun Pian says: Keep the needle in the acupoint for a long period of time without manipulation. It means keeping the needle in the acupoint for a long time and waiting for arrival of qi, known as retention of needle passive.
During the retention period, intermittent manipulations may be done to strengthen the therapeutic effects and for the purpose of strengthening the needle sensation or reinforcing and reducing, known as active retention of needle.
Whether to retain the needle, and how long to retain it depend on the patient’s condition. In general, the needles are retained for 25 to 30 minutes after they have been inserted and manipulated. When treating certain diseases, such as chronic diseases, intractable diseases, pains, spasms, the retention time may be prolonged, during which intermittent manipulations should be done to strengthen the therapeutic effects. When treating certain diseases, such as acute abdominal pain, trigeminal neuralgia, dysmenorrhea, cold symptoms, persistent pain or spastic cases, the retention time may be prolonged to several hours. While treating other diseases, such as cold and fever, needles are withdrawn after they have been inserted and manipulated. There is no need to retain the needle in some cases, such as treating children, blood-letting or quick acupuncture.
5.1.9.2 Withdrawal
Withdrawal refers to taking out or removing a needle after needle retention.
In general, press the skin around the acupoint with the thumb, the index finger and the middle finger of the lefthand, rotate and lift up the needle to the subcutaneous layer slowly and gently with the right hand, then withdraw the needle and press the acupoint with a piece of cotton to prevent bleeding. Finally, check the number of the needles.
5.1 Acupuncture Techniques of Filiform Needle (c)
5.1.10 Management and Prevention of Accidents
5.1.10.1 Fainting During the Acupuncture Treatment
Cause Cerebral ischemia is temporarily caused by nervous tension, weak constitutions, hunger, fatigue, needling done after profuse sweating or bleeding, improper positioning, overly-forceful manipulations done by the practitioner.
Symptom Lassitude, dizziness, pallor, nausea and possibly vomiting, profuse sweating, fluster, cold extremities, sudden drop in blood pressure, a deep, thin pulse, mental disorientation, cyanoticlips and/or nails or sudden loss of consciousness, fecal and urinary incontinence and acrotism.
Management The treatment should be stopped immediately and all needles quickly withdrawn. Assist the patient to lie flat, keep him or her warm and the head slightly lower. In mild cases, the patient will recover
after lying flat for a few minutes and drinking warm or dextrose water. In severe cases, you can needle or pinch Renzhong (GV 26), Suliao (GV 25), Neiguan (PC 6), Shousanli (LI 10); or moxibustion can be done at Baihui (GV 20),Qihai (CV 6), and Guanyuan (CV 4). It is suggested that one perform emergency first aid if necessary.
Prevention During the initial visit for first-time patients, give a detailed explanation of the process of acupuncture, about what it is, how it works and what patients usually experience or can expect during a treatment, in an effort to dispel their fears. A comfortable position should be selected (use supine as much as possible). A minimal number of acupoints should be selected, using slow and gentle manipulations. The patient should not be treated when he or she is hunger or fatigued. There should be an immediate response to any preliminary signs, and in the event that there is an incident, it should be managed quickly, and with a sense of urgency, to nip it in the bud.
5.1.10.2 Stuck Needles
Cause The patient’s mental tension can cause the local muscles to contract tightly around a needle following an insertion. If the intensity of the manipulations is too strong, they can induce local, muscular contractions, or can rotate the needle in only one direction so much that the muscular tissues unduly wrap around the body of the needle.
Manifestation It is difficult for the practitioner to rotate, lift or thrust the needle during manipulations, and withdrawing the needle is also difficult.
Management A practitioner can reduce excessive mental tension by asking the patient to relax. If the stuck needle is caused by rotating the needle in only one direction, twirl it back in the opposite direction to facilitate loosening and unwinding the twisted muscle fibers. In the case of muscular tone, allow the inserted needle to be retained a little longer; then withdraw the needle by twirling. We can also massage around the affected area of the body or insert another needle near the problem area, then withdraw it.
Prevention Nervous patients should be encouraged to relax, and reassured that worrying is unnecessary. Be careful not to insert the needle into a tendon. The twisting angle should not be too large during manipulation. Care should betaken during manipulations to avoid rotating the needle in only one direction.
5.1.10.3 Bent Needles
Cause Unfamiliarity with the anatomical structures associated with the acupoints, inappropriate use of force, needle insertions into the wrong body tissues, and changes in the patients’ body position during insertions; or while the needles are being retained during retention, or inappropriate management of stuck needles can result in a bent needle.
Manifestation The desired direction and angle of the needle’s handle following insertion and retention will be changed, making it difficult to lift, thrust, rotate or withdraw the needle, causing intense pain to the patient.
Management If the needle is only slightly bent, manipulations like lifting, thrusting and rotating etc, should no longer be done. The needle can be slowly withdrawn. However, if the needle has been dramatically bent, it should be slowly withdrawn following the course of the bend. If the bend is caused by the patient changing body position, assist him/her to assume his/her former position, and then slowly withdraw the needle when the surrounding muscles have fully relaxed. It should be noted that it is inappropriate to forcibly withdraw a needle.
Prevention Skillful manipulations are required for all practitioners, which include the flexible application of finger force. Appropriate body position should be selected prior to treatments, and the patient should be instructed not to change his/her position after the needle has been inserted. Also, all areas being treated should be protected so that the handle of the needle wouldn’t be accidentally pressed or pushed by external forces. Bent needles should be properly managed at once.
5.1.10.4 Broken Needles
Cause Poor needle quality can lead to erosion in the body or at the base of the needle; inserting the entire body of the needle below the surface of the skin; inappropriately lifting, thrusting or twirling the needles too strongly during manipulations, causing intense muscular contractions; sudden changes in the patient’ s bodily position during retention and inappropriate management of bent or stuck needles.
Manifestation The needle body is broken during a manipulation with a piece partially left in the body, above or below the skin.
Management The patient should be told to keep calm and remain in the same body position to avoid the remnant from sinking deeper into the body. If the broken end is still protruding from the skin, it should be withdrawn with the fingers or tweezers. However, if it is already beneath the skin, but still visible, press the area of the body surrounding the acupoint perpendicularly, to expose the broken end, and withdraw it with a pair of tweezers. In the event that the broken needle is deeply submerged, it should be surgically removed after locating its position with an X-ray photograph.
Prevention Accidents can be prevented by carefully inspecting needles for quality, and disposing of those that are substandard. The needle for selection should be 0.5 cun longer than desired depth of the point. It should be noted that the needle body should not be completely inserted below the surface of the skin. Part of it should be left outside. In the event of a bent needle, the insertion or manipulation should be stopped, and the needle should be withdrawn immediately. Stuck and bent needles should be properly managed, and never forcibly withdrawn.
5.1.10.5 Hematoma
Cause This may arise from injuries to the skin or the underlying tissue, especially if the tip of the needle is bent or hooked, or from puncturing bloodvessels during insertions.
Manifestation Local swelling, distension and pain after the withdrawal of a needle, followed by the skin around the acupoint punctured turning blue and purplish.
Management A slight hematoma, caused by subcutaneous bleeding, will generally disappear on its own. If the local swelling, distension and pain is severe, or the blue and purplish area is larger enough to restrict or impair motor function and/or movement, management is required. First, a cold compress should be applied to stop the bleeding for several hours, followed by a hot compress or light kneading and massage to the local area to facilitate the dissipation of blood stasis.
Prevention Needles should be carefully inspected before use and practitioners should be thoroughly familiar with human anatomy. It should avoid the bloodvessel when acupuncture.
5.1.11 Acupuncture Treatment Precautions
1. It is inadvisable to give acupuncture to patients who are either hungry, exhausted or nervous. For patients
with weak constitution, or those with severe or chronic illnesses, strong needle manipulation should be avoided. It is preferable if the patient is treated in the supine position.
2. It is contraindicated to needle the points on the abdomen of women who are up to three months pregnant. For those who have been pregnant for more than three months, acupuncture on points of the abdomen or the lumbo-sacral area is contraindicated. Acupuncture is also contraindicated on the following acupoints during pregnancy: Sanyinjiao (SP 6), Kunlun (BL 60), and Zhiyin (BL 67). It can be done for menstrual disorders.
3. Points on the top of the head of infants should not be needled when the fontanels are not closed. In addition, one should not retain the needle for the infants cannot cooperate.
4. Patients with a tendency to bleed spontaneously or who have blood clotting problems should not receive acupuncture.
5. One should not do acupuncture on body areas that have infections, ulcers, scars or tumors.
6. Avoid serious injury to the internal organs. Su Wen·Zhen Yao Jing Zhong Lun says: one should avoid the five viscera when acupuncture the points of the chest and abdomen.
a. Practitionersought to be careful of the angle, direction and depth of needling when needling points around the eyes. Large amplitudes, lifting and thrusting, twirling and rotating or prolonged needle retention are ill- advised, to avoid injuring eyes and bleeding.
b. It is inappropriate to do deep needling on the acupoints above the sides of the 11th thoracic vertebrae on back, the 8th intercostal space level (midaxillary line),and the 6th intercostal space of prothorax (midclavicular line), so as not to stab the heart and lungs. Especially for patients with emphysema, it is possible to injure the lungs, causing a traumatic pneumothorax.
c. It is inappropriate to do deep needling on the acupoints around the flanks and renal regions, so as not to stab the liver, the spleen or kidneys. This is especially for patients with enlargement of liver or spleen. One must be very careful.
d. Practitioners ought to be careful of the angle, direction and depth of needling when needling points around the abdomen of patients with gastric ulcers, intestinal adhesions or intestinal obstructions, and the pubic areas of patients with urinary retention. If inappropriate needling is done on the areas, it is possible to injure the gastrointestinal tract and bladder, causing adverse consequences.
e. One should be careful when needling on the acupoints around the napex and above first lumbar vertebra in the middle of back. It may accidentally injure the medulla oblongata and spinal cord, causing adverse consequences. If deep needling is done in these acupoints, it is easy for electrified sensations to spread toward the limbs or the whole body. Withdraw the needles when this happens. Twirling or rotating the needle is ill-advised.
Appendix: Traumatic pneumothorax
If needling is done on the acupoints around the suprasternal fossae, above the edge of suprasternal notch. The sides of 11th thoracic vertebra level, the 8th intercostal space level (midaxillary line) and the 6th intercostal space of prothorax (midclavicular line), it is possible to injure the lungs, causing a traumatic pneumothorax. The manifestations: In mild cases, the patient will suffer from chest pain and oppression, fluster, and dyspnea; in severe cases, the patient possibly suffer from dyspnea, tachycardia, cyanotic lips, sweating,
and a drop in blood pressure. Physical examination of the injured part of the lung presents a comparatively wide intercostal space; the trachea is even deviated; the lung is resonant to percussion; the breath sounds are obviously reduced or imperceptible; the ipsilateral chest when percussed sounds like a drum; and the cardiac dullness reduced. A chest X-ray will indicate the presence of air in the thorax and a collapsed lung. A diagnosis is made accordingly.
To prevent traumatic pneumothorax when needling, practitioners should be focused and properly positioned to determine and control the appropriate needling angle, direction and depth. If it occurs, preparations should be made to deal with the symptoms, such as medication to stop coughing or infection. In general, the patients can recover on their own after resting for 5-7 days. In severe cases, emergency measures should betaken immediately, such as a thoracocentesis, the insertion of a needle into the chest to aspirate air and reduce the pressure, supply of oxygen, or anti-shock therapy. If the conditions are limited for treatment, one should rescue the patient by transferring the patient to hospital in time.
5.2 Moxibustion
Moxibustion (Jiu) literally means burning. It is a therapy that can prevent and treat diseases with heat stimulation on acupoints or related parts of the body by burning certain combustible materials (mainly refered to as moxa). Moxibustion is a supplementary alternative to acupuncture.
Ling Shu · Guan Neng says if acupuncture cannot be used to treat the disease, moxibustion should be used. Yi Xue RuMen also says that when drugs and acupuncture are inapplicable, moxibustion must be applied. It suggests that moxibustionis a supplementary alternative to acupuncture.
5.2.1 The Functions of Moxibustion
Ben Cao Zheng Yi said that mugwort can warm the twelve meridians to dispel cold, promote the circulation of qi, and dredge the blockage. So moxibustionis widely used, especially for those diseases caused by chronic debilitating disease and wind-cold-wetness evil.
1. Warm and activate meridians, promote qi to activate blood, clear dampness and dispel cold. It can be used in treatment of diseases caused by wind-cold-wetness evil and those caused by qi and blood-insufficiency, such as dizziness, anemia, less milk,amenorrhea.
2. Warm the qi of middle-jiao energy, supporting yang to strengthen the original qi. It has been widely applied to many serious diseases, such as chronic diarrhea, dysentery, enuresis, uterine bleeding, prolapse of the anus, prolapse of the uterus and cold limbs.
3. Remove blood stasis and dissipate pathological accumulation. It has certain curative effect for diseases such as early stages of acute mastitis, scrofula and carbuncle swelling, not festered.
4. Moxibustion of Guanyuan (CV 4), Qihai (CV 6), Zusanli (ST 36) would be beneficial to encouraging the right qi, enhancing disease resistance, preventing disease and staying healthy. In Qian Jin Yao Fang (Valuable Prescription for Emergencies),it says: “The tourists in the country of Wu and Shu should select two or three points for scarring moxibustion and keep the post moxibustion sores unhealed, so as to avoid the malaria and poison gas.”
5.2.2 Classification of Moxibustion
1. Moxibustion with Moxa Cones (Aizhujiu)
Moxa-cones refer to pure moxa wool that has been shaped into small cones while placed on flat surface. (Fig. 5-21) A moxa cone, is also known as a zhuang. Moxibustion with moxa-cones is subdivided into direct and indirect.
a. Direct Moxibustion (Zhi jie jiu): When a moxa cone is placed directly on an acupoint area and ignited, it is called direct moxibustion. It is subdivided into scarring moxibustion, and non-scarring moxibustion.
Non-scarring moxibustion ( Wu ban hen jiu): A moxa cone is positioned on the acupoint and ignited. When about 2/5 of the cone has been burnt, or the patient feels an uncomfortable, burning pain, it should be replaced with another cone. The procedure should be repeated 3-5 times (burning 3-5 zhuang) until the part is red and flushed.
Scarring Moxibustion (Ban hen jiu): It is also known as ”festering moxibusion” . Prior to doing moxibustion, a small amount of garlic juice is applied to the treatment site to facilitate the adhesion and stimulation of the moxa cones on the skin. A moxa cone is then positioned and ignited until it burns completely. In general, this is repeated 5-10 zhuang. It is highly advisable to get the patient’s permission and cooperation prior to using this method, due to the pain, maturation and scar produced in or after the operation. The pain produced following direct moxibustion, can be reduced by gently tapping the skin around the treatment area. Normally, one week after moxibustion, the treatment part will blister and post-moxibustion sores will appear. Five to six weeks later, the sores heal and scars form when the crust falls away.
b. Indirect Moxibustion (Jian jie jiu): This method, also known as moxibustion with material insulation, involves some form of insulation between the cone and the skin, so that there is no direct contact.
Various materials were used for insulation in ancient to treat different kinds of diseases. However, the insulation with animals, plants and minerals belongs to traditional Chinese medicine in most cases. Due to different diseases and symptoms, there are unilateral and compound medicines. This method has special therapeutic effect for both playing the role of moxibustion, and the function of drugs.
Ginger Moxibustion (Ge jiang jiu): Fresh ginger is cut into slices, each about 2-3 cm wide and 0.2-0.3 cm thick. Several needle holes are then punched into the slices that are then placed on the acupoints /areas selected. The moxa cone is then placed on top of the ginger slice where it is ignited and burned. It is usually repeated 5-10 zhuang. This method is indicated for symptoms related to cold for the functions of relieving exterior syndromes and expelling cold, warming the middle and stopping vomiting. Thus, it is indicated for symptoms such as exterior syndromes, abdominal pain, diarrhea, spermatorrhea, premature ejaculation, sterility, dysmenorrhea,anemofrigid- damparthralgia.
Garlic Moxibution (Ge suan jiu): Garlic cloves are cut into slices, about 0.2-0.3 cm thick, and then holes are punched into them. The garlic is then placed on the acupoints/areas selected and moxa cones are ignited and burned on top of them. It is usually repeated 5-7 zhuang. Garlic liquid irritates the skin, causing bubbles after moxibustion. If you do not want to make the bubble, move the garlic slice appropriately. Garlic moxibustion can clear away the heat evil or detoxify, and has a pesticide function. Thus, it is indicated for symptoms, such as pyocutaneous that has not fester, poisonous insect bite, asthma, umbilical tetanus, phthisis, scrofula.
Long Snake Moxibustion (assisted moxibustion): This method refers to the assisted moxibustion of dressing mashed garlic on the back along Dazhui (GV 14) to Yaoshu (GV 2).
Salt Moxibustion (Geyan jiu): This method is usually done on the navel. First, the navel is filled with salt to the level of the skin, or with ginger insulation, followed by placing a large-sized moxa cone on top of the salt; it is then ignited and burnt. When consumed, the ashis removed, and it is replaced with another until all the cones required have been consumed. It is usually repeated for 5-9 zhuang. Salt moxibustion has the function of warming the middle and expelling cold, supporting yang to strengthen the original qi. Thus, it is indicated for symptoms, such as acute cold vomiting, diarrhea, abdominal pain, collapse and postpartum anemic fainting.
Monkshood Cake Moxibustion (Fu zi bing jiu): A cake or a slice of monkshood (it is made of monkshood powder mixed with alcohol, shaped like a coin, and punched with several holes) is placed on the affected area where moxa cones are placed on top of it to be ignited and burnt.
Due to the monkshood’s warm nature and its effect of warming the kidneys to invigorate yang, it is adopted to treat impotence, spermatorrhea, premature ejaculation, and ruptured abscesses resistant to healing caused by decline of vital gate fire.
2. Moxibustion with Moxa Sticks (Ai tiao jiu)
Moxa sticks are made in the following manner: Tightly roll 24 grams of soft, pure moxa wool with a sheet of soft, thin paper (26 cm by 20 cm). Roll it into a column of approximately 1.5 inches in diameter, and then wrap it with soft, tough, mulberry paper. A medicinal herbal moxa stick is made by combining other drug powders.
A medicinal herbal moxa stick prescription: Combine 6 grams each of the following special ingredients, and pound them into powder: cinnamon, ginger, clove, asarum, angelica, radix Aucklandiae, rhizoma Atractylodis, realgar, myrrh, frankincense, etc.
Moxibustion with moxa sticks has two varieties: Mild moxibustion ( Wen he jiu) and pecking moxibusiton (Que zhuo jiu). (Fig. 5-22)
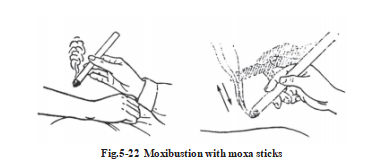
a. Mild moxibustion ( Wen he jiu): One end of a moxa stick is ignited and held over an acupoint/area. The distance between the end of the stick and the skin should be about 4 cm. The intention here is to bring warmth to the treatment area. The patient should not feel any burning sensations. Each acupoint/area should receive moxibustion until the part is red and flushed.
b. Pecking Moxibusiton (Que zhuo jiu): With this method, the distance between the ignited end of a moxa stick and the patient’s skin is not fixed. As its name indicates, it is moved up and down over the point/area like a pecking bird.
3. Warm-Needle Moxibustion ( Wen zhen jiu)
It is actually a combination of acupuncture and moxibustion. This method is used when both retaining needles and moxibustion are available. During the manipulation, after arrival of qi, while the needle is still retained in the point,affix the moxa holding tight by finger or a small section of moxa stick (about 1-2 cm long) on the needle’s handle, and then ignite it, so that the heat enters the body through the needle body. When the moxa or moxa stick burns out, remove the ashand take out the needle (Fig. 5-23). Usually moxa stick is about 4 cm away from skin.
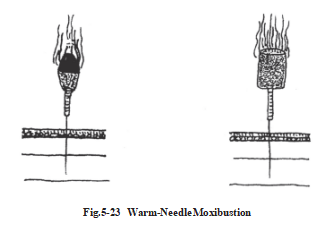
5.2.3 Precaution
5.2.3.1 Order of Moxibustion
Qian Jin Yao Fang (Invaluable Prescriptions for Emergencies) records that moxibustion ought to be conducted on the yang aspect first, followed by theyin; and the upper area first, then the lower. Clinically, we should start moxibustion from the upper part of the body, going on to the lower part; first head and body, then limbs. However, in special circumstances, these rules can be modified to coincide with the patient’s condition.
5.2.3.2 Moxibustion Contraindication
a. Whenever doing moxibustion, practitioners should take precautions to prevent the fire from the moxa from burning the skin or clothes.
b. In principle, patients with excess syndromes, heat syndromes or fevers due to yin deficiency are contraindicated for moxibustion.
c. Scarring moxibustionis not allowed on the face or head, nor on areas close to large bloodvessels.
d. Moxibustion is prohibited on the abdomen and lumbo-sacral areas during pregnancy.
5.2.3.3 Moxibustion Disposal
Following moxibustion the local skin area will appear red or flushed, accompanied by a scorching, hot sensation; this is a normal phenomenon, and no management is required. However, blisters will appear if moxibustionis excessive or prolonged; if not ruptured, they will be absorbed naturally. Large blisters can be lanced and drained or the fluid inside the blisters can be aspirated with a hypodermic needle, followed by the application of gentian violet and a bandage. When scarring/festering moxibustionis done, during the suppurative stage of the sores, patients should be informed about the importance of proper rest, keeping the affected area clean and dressed to protect the sores and prevent infection until they are healed. In the event that the resulting sores are not properly attended to, they may ooze kelly pus and blood, which can be treated by practitioners with anti- inflammatory ointments or rub-in ointment.
5.3 Cupping Therapy (Ba Guan Fa)
Cupping therapy, also known as “horn method (Jiaofa)” in ancient China, is a treatment in which a cup (Guan) is attached to the skin with suction to cause local blood congestion for disease treatment and prevention.
Cupping therapy was primarily used to drain stagnant blood and pus. However, with medical progress, not only have the materials and methods of cupping therapy improved, but the scope of its indications has also greatly increased. Clinically, it is often employed in conjunction with acupuncture and moxibustion.
5.3.1 Type of Cups
There are several types of materials commonly used and they are bamboo cups (Zhu guan),pottery cups (Tao guan),glass cups (Bo li guan) and plastic suction cups or air-withdrawing cups (Chou qi guan), etc. (Fig. 5-24)
The bamboo cups are light and economical, and suitable for boiling, but have the drawback that they are prone to crack from dryness, which causes air leakage and weakens their suctioning force. The pottery cups have strong suction, but they are heavy and prone to smash. The glass cups are transparent to help to observe the skin in the cup and the quantity of blood extracted. But they are also prone to break. Some suction cups
are made of plastic. They are easy to carry and widely used.
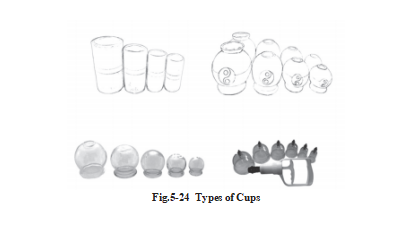
5.3.2 Method of Creating Suction Inside the Cup
The methods of creating suction inside the cup can be divided into the fire-suction method (Huo guan fa), the water-suction method (Shui xifa), and the suction cup method (Chou qifa), and they can be explained as follows:
The fire-suction method is a method to create negative pressure by introducing an ignited material inside the cup to consume the air, thereby making the cup suck itself onto the skin. The following details pertain to different ways of creating suction using fire: the fire-twinkling method (Shan huofa), the fire-throwing method (Tou huo fa), the cotton-sticking method (Tie mian fa), the fire-throwing method (Jia huofa), the alcohol-firing method (Di jiu fa). The first two are commonly used.
1. Fire-Twinkling Method (Shan huofa): Light an alcohol soaked cotton ball, held with a clamp or forceps or using a strip of paper, place it inside the cup, swirl it around inside one circle, take it out immediately and press the cup on the selected area. The cup will attached itself to the skin. Caution should betaken to avoid scalds or burns by not over-heating the mouth of the cup. (Fig. 5-25)
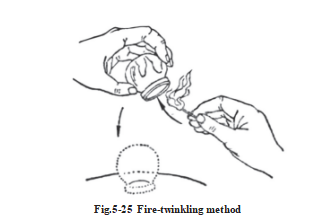
2. Fire-Throwing Method (Tou huofa): An alcohol soaked cotton ball or a piece of paper is ignited and placed inside the cup. After a short time, quickly press the cup against the skin on the desired location. It is often applied to the lateral side of the body. (Fig. 5-26)
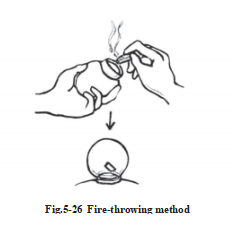
5.3.3 Application of cupping
One can choose different cupping methods according to the patient’s condition.
5.3.3.1 Cup-Retention Method (Liu guan fa)
It involves keeping the cup on the selected location for 3-5 minutes before removal. This method is commonly used in clinic to treat general diseases.
5.3.3.2 Mobile/Moving Cupping (Zou guan fa)
This is also known as “sliding cupping” . The lubricant should be applied to the skin over the treatment area prior to using this method to reduce pain. Once suction has been created, the cup is held and slid across the skin until it becomes rosy and congested, or even blood stagnation is seen. It is suitable for treating large, thickly- muscled areas and treating the excess diseases. (Fig. 5-27)
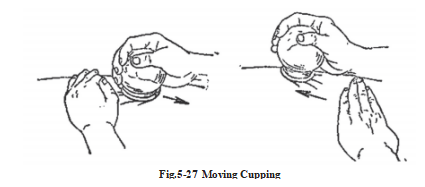
5.3.3.3 Flash Cupping (San guan fa)
This method is done by rapidly placing and removing the cup repeatedly over the same place until the skin turns rosy.
5.3.3.4 Needle-Retention Cupping (Liu zhen ba guan)
This method is done by applying a cup over the center of the place where a needle has been inserted. (Fig. 5-28)
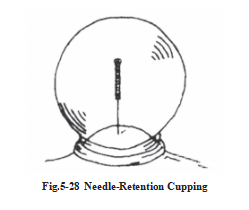
5.3.3.5 Pricking and Cupping Therapy (Ci xue ba guan)
This is also referred to as collateral-pricking and cupping. It can draw out poison and clear heat, and strengthen the treatment of pricking blood therapy.
5.3.3.6 Medicinal Cupping (Yao guan)
There are actually two methods involved here: boiling medicinal cupping and reserving medicinal cupping.
5.3.4 Action and Indication for Cupping
Cupping therapy has the effect of warming the meridians, invigorating qi and blood circulation, relieving blood, alleviating pain and swelling and dispelling damp and cold. With this extensive range of indication, it’s commonly applied for wind cold-damp bi syndrome, various nerve paralysis, acute and chronic pains, and dysfunction of the zang and fu organs. In addition, for surgical diseases such as erysipelas, venomous snakebite it can also be used.
5.3.5 Cup Removal and Precaution
1. Cup Removal: When removing a cup, it should beheld in one hand, while the other hand presses the skin around the mouth of the cup, to break the seal created by the suction. In this way, the air islet in and the cup is released. One should avoid lifting or rotating the cup strongly. (Fig. 5-29)
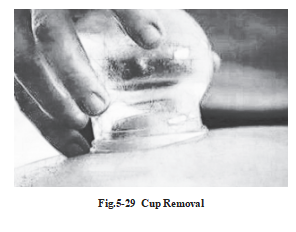
2. Precaution
a. Patients should be comfortably positioned. It should be noted that cups are prone to drop off, if part of the skin and flesh wrinkles, loosens, or in case of uneven scar area or body moving.
b. The size of the cup used is determined by the cupping location. Action must be quick and strong.
c. Precautions should betaken to avoid scalding the skin. If using the fire-twinkling method, the cotton should not be soaked with too much alcohol, to prevent the alcohol from dripping down the skin. If using the fire- throwing method, the action should be quick. Since there is burning material inside the cup, which is apt to drop down and burn the skin, it is often applied with the mouth of the cup upward. The treatment of blisters has much in common with moxibustion.
d. Cupping is contraindicated on patients with skin allergies, ulcers, oedema, as well as on the sites near large bloodvessels. It is also contraindicated for those that have high fevers accompanied by convulsions, and on the abdominal and sacral areas of pregnant women.
5.3.6 Disinfection of Cupping Equipment
The cups can be disinfected in different ways to prevent cross infection. For disinfecting the cups, generally it is necessary to wear one-time sterilized disposable gloves. Disposable gloves must be changed each time. before, during, and after the cups’ disinfection.
5.3.6.1 Glass Cups (Bo li guan)
1. Disinfection for Commonly Used Glass Cups
a. After high pressure autoclave sterilization, or boiled with cleaning agent for 10 minutes or more, the cups should be washed with running water and dried with clean paper towels before use.
b. You can use water of sodium dichloroisocyanurate (C3Cl2N3NaO3) and Trichlorinafed isocyanuric acid (C3Cl3N3O3) or bleach containing available chlorine of 6,000 mg/L (15 tab per kg of water ), to soak for 30 minutes, rinse with running water and drain water off for dryness or dry cups with cleaning paper towels, and then use 75% alcohol for wiping cups for 1 minute (wipe twice, each time wiping for 30 seconds, a total of 1 minute). Before using, burn the mouth of cups two times.
2. Disinfection for Glass Cups Contaminated by Blood: If there is blood or tissue fluid or body fluid, the doctor must wear gloves while doing disinfection. Washing the blood off with running water is a very important prior process before next procedure.
a. After cleaning off the blood with running water, use high pressure autoclave sterilization, or use the cleaning agent to boil cups for 20 minutes or more, and then rinse them with running water and dry them with clean paper towels before use.
b. Wear disposable gloves to wash the blood off with running water, then use water of sodium dichloroisocy anurate(C3Cl2N3NaO3) and Trichlorinafed isocyanuric acid (C3Cl3N3O3) or bleach containing available chlorine of 10,000 mg/L (25 tab per kg of water ),soak for 60 minutes,rinse with running water and drain water off; or dry cups with cleaning paper towels, and then use 75% alcohol for wiping cups for 1 minute (wiping twice, each time 30 seconds, for a total of 1 minute). Before using, burn the mouth of cups two times.
5.3.6.2 Disinfection for Suction Cups or Air-Withdrawing Cups
Each patient uses his or her own air-withdrawing air cups, rinses them with running water to get rid of the blood firstly after each use, and places them in a plastic bag. Patients must immerse them in 75% alcohol for at least 20 minutes after returning home, and then place them into a clean bag for future use. Practitioners must wear disposable gloves to do air-withdrawing cupping job each time.
5.3.6.3 Disinfection for Bamboo Cups (Zhu guan)
Washoff the blood with running water firstly, boil the bamboo cups with cleaning agent for 20 minutes or more, then wash with running water and dry the cups with clean paper towels before use.
5.3.6.4 Disinfection for Non-Heat Resistant Plastic Cups, Rubber Cups (polyethylene, polystyrene)
After cleaning off the blood with running water, drain the water off, soak in a solution of 1% (10,000 mg/L) peracetic acid for 60 minutes, then rinse with running water and drain the water off for dryness.
5.3.6.5 Disinfection for Pottery Cups (Tao guan)
After cleaning, boil with cleaning agent for 20 minutes or more, then wash with running water and dry the cups with clean paper towels before use.
5.4 Three-Edged Needling Therapy, Skin Needling Therapy, Electro- Needling Therapy and Point Injection Therapy
5.4.1 Three-Edged Needling Therapy (San leng zhen fa)
The three-edged needle was known as the “sharp needle” in ancient times. This therapy involves pricking certain areas of the skin to discharge blood or serous fluid. (Fig. 5-30)
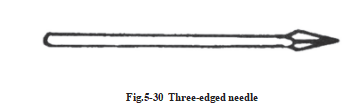
5.4.1.1 Manipulation Method
1. Spot Pricking Method (Dian cifa): This method is done by creating a slight wound with quick, vertical, superficial pricking with a needle. Then withdraw the needle quickly. Disinfect the site. Press the skin to create local hyperemia. Prick the acupoint quickly, then squeeze the puncture hole to do for a little bloodletting. Finally, press the punctured hole. This method is usually applied to acupoints on extremities, such as Twelve Wells (Shi er jing xue), Shixuan (EX-UE 11) andErjian (EX-HN 6). (Fig. 5-31)
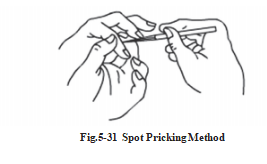
2. Scattered Pricking Method (San cifa): This method is also known as the “Leopard print pricking” . It is used to slightly prick a small area around an affected part with a three-edged needle. Needle pricks can be made in the form of a ring around the outer margin to the center of affected part to dissipate swelling, dispel blood stasis, so as to facilitate healing and remove blockages in the meridians. This method is usually used for local blood stagnation,haematoma, edema, stubborn dermatitis, etc. (Fig. 5-32)
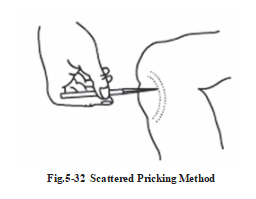
3. Collateral Pricking Method (Ci luofa): It is a method to prick the vein to let out sufficient blood. This method helps to expel the stagnant blood and reduce the harmful pathogenic factors, which is usually used on acupoints such as Quze (PC 3) and Weizhong (BL 40) for the treatment of acute vomiting and diarrhea, sunstroke and fever. (Fig. 5-33)
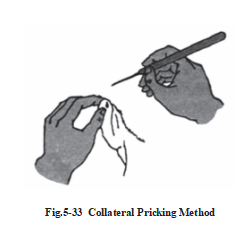
4. Open Picking Method (Tiao cifa): Hold the handle of the needle with the needling hand and swiftly prick the skin. Then discharge a small amount of blood or serous fluid. Another method is to prick it about 5 mm deep, then tilt the body of the needle and tease the tip of the needle to rupture the subcutaneous fibers. This method is stimulating, which is commonly used to treat diseases, such as vascular headache, asthma, insomnia, stomach pain, scapulohumeral periarthritis and cervical vertebra.
5.4.1.2 Indication
Three-edged needle therapy is mostly used for removing blockages in the meridians, opening the orifices, clearing heat, regulating qi and blood, dissipating swellings and relieving pain. Its extensive indications include excess syndromes, heat syndromes, blood stasis and various pain syndromes.
5.4.1.3 Precaution
a. Strict disinfection must be applied to the area to be pricked to prevent infection.
b. For spot pricking, the operation should be light, steady, exact and rapid. Deep insertion and excessive use of force should be avoided to prevent deep large artery damage.
c. Pricking should never be done on patients with weak constitution, anemia, hypotension, angioma, pregnant or procreative women, or on individuals who are susceptible to bleeding.
d. Patients should be placed in a comfortable position to prevent faint during this procedure.
e. Treatments are given once a day or every other day. A course of treatment includes 1 to 3 treatments. To avoid massive bleeding, 1 to 2 treatments a week is appropriate. The quantity of bleeding depends on the patient’s condition, but generally, 3-5 ml every time is appropriate.
5.4.2 Skin Needling Therapy (Pi FuZhen Fa)
Skin needling is also called “plum-blossom needle” or “seven-star needle”, which is a needle consisting of stainless steel needles to tap the body or acupoints. Skin needling therapy originated from “Half Needling (Ban ci)”, “Skin Needling (Mao ci)” and “Centro-Square Needling (Yang ci)” in ancient times. Cutaneous needling is used for preventing and treating diseases by tapping on the cutaneous regions to promote the smooth flow of qi in the meridians and regulate the functions of the zang and fu organs. (Fig. 5-34)
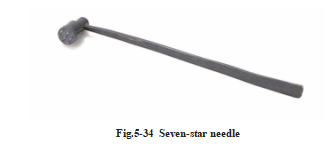
5.4.2.1 Manipulation Method
1. Tapping Location: In general, there are 3 different tapping locations: tapping along the meridians, on the acupoints and on local areas.
2. The Intensity of Stimulation and Course of Treatment: Generally, it is classified into the following 3 categories: light tapping (Qing ci),heavy tapping (Zhong ci) and moderate tapping (Zhong ci).
a. Light Tapping (Qing ci): Light tapping is done until the skin becomes flush and congested; this is used on head and face, and is advisable for elderly, weak or female patients, as well as patients with deficiency syndromes or those requiring extensive treatments.
b. Heavy Tapping (Zhong ci): Heavy tapping is done until the skin becomes apparently flush and is slightly bleeding. This method is commonly applied to tender points on the back and buttocks area of strong, young patients,and those with excessive syndromes or acute outbreaks.
c. Moderate Tapping (Zhong ci): Medium-strength tapping is done somewhere between light and heavy stimulation, until the skin becomes relatively flush but not bleeding, which is advisable for general locations and general patients.
Treatments are given once a day or every other day; 10 days, treatments comprise 1 course.
3. Manipulation
a. Tapping Method (Kou ci): After the routine sterilization on needles and the tapping area, hold the handle with the thumb, middle and ring fingers of the needling hand at the end of handle near the posterior portion of palm. Extend the index finger to apply pressure to the middle section of handle and place the head of needle directly over the skin. Tap the skin with the needle tip in a loose, flexible movement of the wrist, then rebound up immediately, and continue repeatedly tapping in this manner.
b. Roller Pricking (Gun ci): Use the specially-made roller needle and rollback and forth over the skin.
5.4.2.2 Indication
There is a very wide range of applications for cutaneous needling. Every clinical syndrome can be used.
5.4.2.3 Precaution
a. The needles should be frequently inspected. The tips of the needles should be even and free from hooks. Roller needles should be flexible.
b. Tapping manipulations should be swift and gentle. Needle tips should descend perpendicularly, avoiding oblique angles, clawing or teasing, which will cause more pains.
c. Tapping should never be applied to areas with ulcer, traumatized tissue, acute infectious disease or acute abdomen.
d. The local skin surface should be cleaned and sterilized to prevent infection after heavy tapping on local areas or acupoints that results in bleeding.
e. Roller needling is inadvisable on bony prominences to avoid pain or bleeding.
5.4.3 Electro-Needling Therapy (Dian Zhen Fa)
Electrotherapy combines needling and electrical stimulation by sending a small electric current through the needle after insertion and arrival of qi, to prevent and treat diseases.
5.4.3.1 Manipulation Method
1. Point Prescription: The selection and organization of acupoints for electrotherapy is the same as for filiform needling therapy. It is advisable to select 1-3 pairs of acupoints on the same side, then the main points combine with the corresponding auxiliary points for electrotherapy after arrival of qi. The selection of acupoints can be free. Some people argue for choosing acupoints through the nerve stem.
2. Electrotherapy Manipulation: Adjust the output potentiometer to “0”, then connect the cathode outlet to the principal acupoint, and the anode to the assistant point. If an option is without differentiation between cathode and anode, just connect the two outlets to the handles of two needles respectively. Switch the power supply on, and select the required waveform; then adjust the output current from smaller to larger until you have a suitable size. Generally, the current time is 5-20 minutes for each treatment.
3. Electrical Current Stimulation Intensity: Generally, the current intensity between the threshold of sensation and threshold of pain is the optimal one. To a certain intensity, the patient would have the sensation of numbness, but no pain. It is advisable to set the current intensity according to the patient’s tolerance.
5.4.3.2 Actions and Indication
Electro-Acupuncture has the function of adjusting human body’s physiologic function, calming, promoting blood circulation, and adjusting the muscle tension, etc. The actions and indications of electrotherapy are as extensive as those of filiform needling therapy. It can be used to treat various diseases, such as different kinds of pain syndrome, bi syndrome, dysfunction of heart, stomach, intestine, and damage to muscles, ligaments and joints.
The actions of electro-acupuncture are different depending on the waveform and frequency: (Fig. 5-35)
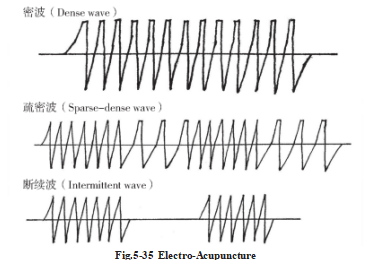
1. Dense Wave (Mi bo): frequency: 50-100 times/sec. It reduces nervous stress function and tends to inhibit sensory and motor nerves. So it is commonly used for pain relief, sedation, remittance of spasms in muscles or vessels, and acupuncture anesthesia, etc.
2. Sparse Waves (Shu bo): frequency: 2-5 times/sec. Its stimulating effect is strong, and can cause muscle contraction and enhance the tension of muscle ligament. The sparse wave stimulates sensory and motor nerves with short-term usage, so it is usually used for various impairments of muscles, joints, ligaments, or tendons, as well as various syndromes.
3. Sparse-Dense Wave (Shu mi bo): This waveform automatically alternates from sparse to dense wave. The single waveform is susceptible to adaptation, and this defect could be retrieved by sparse-dense waveforms. Its main therapeutic effect is excitation, which promotes metabolism, circulation of qi and blood, improves the nutrient supply to tissues, and acts to eliminate inflammatory edema.
4. Intermittent Wave (Duan xu bo): This is a wave that is regularly interrupted and automatically continues. It is free from adaptive tendencies and its motive power is strong to enhance the excitation of striated muscle tissue. It is usually used to treat flaccidity and paralysis.
5. Sawtooth Wave (Ju chi bo): It is also called respiratory wave, whose frequency is close to the law of human breathing. It is commonly used in the treatment of respiratory failure, but not acupuncture.
5.4.3.3 Precaution
a. Needle fainting should be prevented. Since electrical stimulation is relatively strong, it is inadvisable for patients who are nervous or have weak constitutions.
b. When adjusting the electric current, sudden increases should be avoided to prevent sudden and/or intense muscular contraction which could result in bent or broken needles.
c. After warming needle moxibustion, the needle handle may be burnt, and its surface oxidized, which will cause it to lose electrical conductivity. The output wire should beholding the needle body.
d. Avoid passing the electric current through the heart for patients with heart disease. It is usual to connect the same pair of output electrodes to the same side of the body. When electrotherapy is used near the chest or back, do not connect the two electrodes across both sides of the body. When electrotherapy is used near the medulla oblongata or spinal cord, the electric current should have small wavelengths with low intensities, to prevent accidents. Precautions should betaken with pregnant women when using electrotherapy.
5.4.4 Point Injection Therapy (Xue Wei Zhu She Fa)
This therapy incorporates the comprehensive effect of treating diseases by combining the actions of medicine with acupuncture. It can not only play the role of acupuncture points, but also the pharmacological action of drugs.
5.4.4.1 Manipulation Method
1. Apparatus: Injector, injection.
2.Acupoint Selection: The principles concerning acupoint selection are the same as those of filiform needling therapy. However, with this therapy, local positive, sensitive spots (trigger points) are usually chosen by palpation on the meridians or acupoints, only 2-4 points for each treatment.
3. Injection Dosage: Dosages should not exceed those given in the instructions and suggested by the manufacturer. The amount of injection is also very different according to different points.
4. Manipulation: Slowly depress the needle until the tip reaches the proper depth; when the patient feels the needling sensation, and there is no blood in the syringe after drawn, inject the liquid medicine into the point just the same as for an intramuscular injection.
5.4.4.2 Indication
This therapy can be used in almost all the diseases that are suitable for acupuncture treatment.
5.4.4.3 Commonly Used Medicine
All liquid medicines used for intramuscular injections can be used for point injection. However, the appropriate medicine should be selected according to the pathological condition and the medicinal property.
5.4.4.4 Precaution
a. Before treatments, patients should be informed about the normal reactions of this therapy.
b. Strict aseptic technique should be observed to prevent infection.
c. Attention should be paid to the nature, pharmacological action, dosage, incompatibility, side effect and allergic reaction, etc, of medications. Hypersensitivity tests are necessary towards medicines which might possibly produce allergic reactions. It can be used if the hypersensitivity test shows negative.
d. To avoid accidents,fluid medicines should not be injected into the articular cavities, spinal canals or blood vessels. In addition, injections into nerve stems should be avoided, to prevent injuries to nerves.
e. Pregnant women are at risk of aborting if the injections are received in the lower abdomen or lumbo- sacral area, and points such as Sanyinjiao (SP 6) and Hegu (LI 4). Also, fluid dosages should be decreased and fewer acupoints selected for elderly individuals and the ones with weak constitutions.
5.5 Scalp Acupuncture (Tou zhen)
Scalp acupuncture therapy involves needling specific stimulation areas of the scalp for the prevention and treatment of disease. It originated from two theories, the theory of traditional zang-fu organs and meridians and the projection area of cortical functional localization on the scalp. Corresponding scalp lines were then defined based on these theories.
Scalp acupuncture is universally employed in clinic at present. There are different scalp acupuncture points named systems, such as Fang Yun-peng (Shanxi), Tang Song-yan (Shanghai), Jiao Shun-fa (Shanxi), Lin Xue-jian (Shanghai) and Zhu ming (Beijing). In order to adapt to the international spread and exchange of information on scalp acupuncture therapy and to facilitate its development, the Chinese Acupuncture Academy has formulated a “Standard Scalp Acupuncture Nomenclature” . Although each system is varied, the operation methods, the scopes of adaptation, and the attentions to other issues are basically the same. The following contents state about this.
5.5.1 Standard Scalp Acupuncture Location and Indication
1. Frontal Mid-Line (MS 1): forehead area, 1 cun in length from Shenting (GV 24 or DU 24) of governor
meridian, straight down along the meridian.
Indications: epilepsy, mental disorder, rhinopathy, etc. (Fig. 5-36)
Billingual Acupuncture and Moxibustion
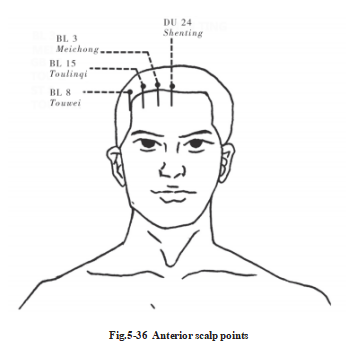
2. Frontal Lateral-Line1 (MS 2): forehead area, 1 cun in length from Meichong (BL 3), straight down along the meridian.Indications: coronary heart disease, angina, bronchial asthma, bronchitis, insomnia, etc. (Fig. 5-36)
3. Frontal Lateral-Line2 (MS 3): forehead area, 1 cun in length from Toulinqi (GB 15), straight down along the meridian.Indications: acute and chronic gastritis, gastric and duodenal ulcers, liver and gallbladder diseases, etc. (Fig. 5-36)
4. Frontal Lateral-Line3 (MS 4): forehead area, 1 cun in length from the point 0.75 cun medial to touwei (ST-8) straight down.Indications: functional uterine bleeding, impotence, seminal emission, uterine prolapse, urinary frequency, urgency, etc. (Fig. 5-35)
5. Vertex Mid-Line (MS 5): vertex area, from Baihui (GV 20) of governor meridian to Qianding (GV 21) along the midline of the head (1.5 cun).Indication: disorders of the lower back, legs and feet (e.g. paralysis, numbness or pain), cortical hyperdiuresis,anal prolapse, hypertension, vertex pain, etc. (Fig. 5-37)
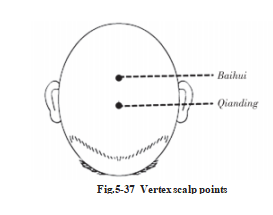
6. Anterior Vertex-Temporal Oblique Line (MS 6): vertex area and cephalic region. From Qianshencong, one of the acupoints of Sishencong (EX-HN 1), obliquely to Xuanli (GB 6).
Indications: this entire line is divided into 5 equal parts. The upper 1/5 is used for treating paralysis on the contralateral lower limb and trunk. The middle 2/5 are for paralysis of the upper limb. The lower 2/5 are for central facial palsy, ataxia aphasia, salivation, cerebral atherosclerosis. (Fig. 5-38)
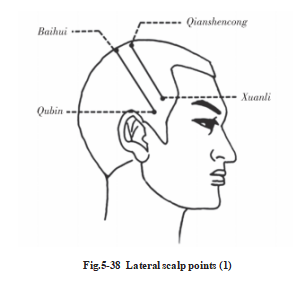
7. Posterior Vertex-Temporal Oblique Line (MS 7): vertex area and cephalic region, 1 cun posterior and parallel to the anterior oblique line of vertex-temporal. From Baihui (GV 20) obliquely to Qubin (GB 7).Indications: This entire line is divided into 5 equal parts. The upper 1/5 is used for treating abnormal feeling in contralateral trunk and lower limbs. The middle 2/5 are for abnormal feeling in the upper limb. The lower 2/5 are for abnormal feeling on the head and face. (Fig. 5-38)
8. Lateral Vertex Line1 (MS 8): vertex area, 1.5 cun lateral to governor meridian, 1.5 cun in length posterior to Tongtian (BL 7) along the meridian.Indications: disorders of the lower back and legs, e.g. paralysis, numbness and pain. (Fig. 5-39)
9. Lateral Vertex Line2 (MS 9): Vertex area, 2.25 cun lateral to governor meridian, 1.5 cun in length from Zhengying (GB 7) to Chengling (GB 18).Indications: impairment of the shoulders, arms and hands, such as paralysis, numbness and pain. (Fig. 5-39)
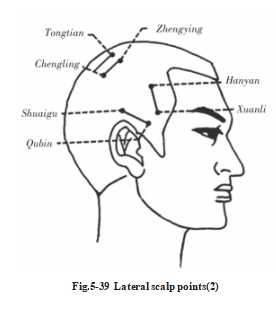
10. Anterior Temporal Line (MS 10): temporal area, from Hanyan (GB 4) of Gall Bladder Channel of Foot- Shaoyang to Xuanli (GB 6).Indications: migraine, tinnitus, deafness, vertigo, etc. (Fig. 5 39)
11. Posterior Temporal Line (MS 11): temporal area, from Shuaigu (GB 8) of Gall Bladder Channel of Foot- Shaoyang to Qubin (GB 7).Indications: migraine, tinnitus, deafness, vertigo, etc. (Fig. 5-39)
12. Upper Occipital Mid-Line (MS 12): occipital area, from Qiangjian (GV 18) of governor meridian to Naohu (GV 17), 1.5 cun in length.Indications: eye disease, foot ringworm. (Fig. 5-40)
13. Upper Occipital Lateral Line (MS 13): occipital area, 0.5 cun lateral and parallel to the upper-mid-line of the occiput.Indications: cortical visual disorders, cataracts, myopia. (Fig. 5-40)
14. Lower Occipital Lateral Line (MS 14): occipital area, 2 cun in length from Yuzhen (BL 9) of urinary bladder meridian straight down.Indications: balance disturbances resulting from diseases of the cerebellum, occipital pain. (Fig. 5-40)
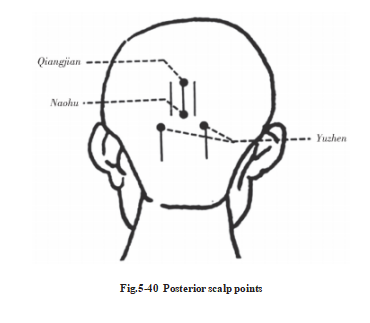
5.5.2 Indication for Scalp Acupuncture Therapy
Scalp acupuncture therapy is often used clinically to treat cerebral diseases. Other common or frequently occurring diseases, such as headaches, trichomadesis, hypertension, oculopathy, rhinopathy, and a variety of painful diseases can also be treated with scalp acupuncture therapy.
5.5.3 Manipultaions Method
1. Position: Sitting or lying.
2. Insertion: Insert the needle quickly into the skin at a 30° angle until the force of the resistance felt by the manipulating fingers diminishes. Hold the needle parallel to the scalp and continue to twirl it until it reaches an appropriate depth.
3. Manipulation: Generally, the needle handle is held with the thumb pad and the radial aspect of the index finger. Twist the needle by rapidly and continuously flexing and extending the metacarpophalangeal joint of the index finger. The twisting speed should be approximately 200 times/minute. Twist the needle continuously for 2-3 minutes, then retain the needle for 20-30 minutes. The needle retention time may be extended depending on the pathological condition. Some patients with stroke can retain the needle for long hours.
4. Needle Withdrawal: Pressure should be applied to the insertion hole for 1-2 minutes to prevent bleeding following the withdrawal, for the head bleeds easily.
5.5.4 Precaution
a. Appropriate aseptic techniques must be employed to prevent infection.
b. Prevent needle fainting.
c. Scalp acupuncture therapy is inadvisable for infants since their fontanels have not yet closed.
d. Scalp acupuncture is inadvisable for patients during the acute stages of a hemorrhagic stroke, when they are in coma or their blood pressure is too high. Once these conditions have stabilized, treatment with scalp acupuncture can begin. However, scalp acupuncture should be used as early as possible for patients with hemiplegia due to cerebral infarction (ischemic strokes). Scalp acupuncture should be used cautiously in cases where patients have complications such as high fever, acute inflammation or heart failure.
5.6 Ear Acupuncture Therapy (Er Zhen)
Ear acupuncture therapy treats and prevents diseases by stimulating certain points on the auricles with needles or by other methods. This therapy can not only treat disease, but is also used as a diagnostic indicator for disease.
5.6.1 Auricular Surface Anatomy (Fig. 5-41)
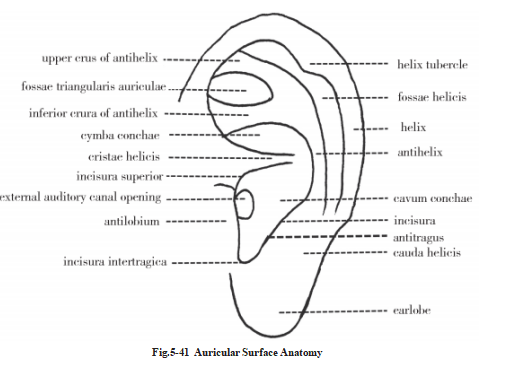
5.6.2 Auricular Point Distribution
Points located on the lobe are related to the head and facial region, those on the scapha to the upper extremities, those on the antihelix and its two crura to the trunk and lower extremities, those in the cavum and cymba conchae to the organs. (Fig. 5-42)
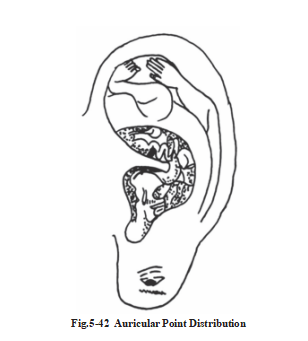
5.6.3 Auricular Point Location and Indication (Fig. 5-43)
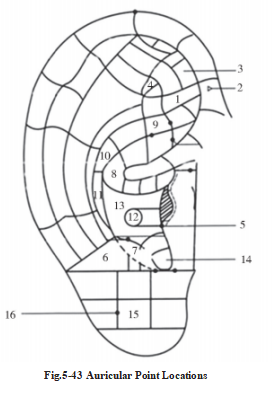
1. Sciatic Nerve: anterior 2/3 of the inferior crus.
Indications: sciatica, paralysis of the lower extremities.
2. Sympathetic: junction between the terminus of the inferior crus and the inner border of the helix.
Indications: gastrointestinal spasms, angina, biliary colic, ureterolithiasis, functional disturbances of the
automatic nervous system.
3. Internal Genitalia: the inferior part of the anterior 1/3 of the triangular fossa.
Indications: dysmenorrhea, reproductive system diseases such as menstrual disease.
4. Ear Shenmen: the superior part of the posterior 1/3 of the triangular fossa.
Indications: insomnia, excessive dreaming, withdrawal syndrome, epilepsy, hypertension, neurasthenia.
5.Adrenal Gland: top of the lower eminence of the tragus.
Indications: hypotension, rheumatoid arthritis, mumps, dizziness, asthma, shock, etc.
6. Occiput: posterior portion of the lateral surface of antitragus.
Indications: dizziness, headache, epilepsy, asthma, neurasthenia, etc.
7. Subcortex: medial surface of the antitragus.
Indications: dysmenorrhea, neurasthenia, insomnia, etc.
8. Stomach: end of the helix crus.
Indications: gastro spasm, gastritis, gastric ulcer, insomnia, toothache, indigestion, etc.
9. Kidney: posterio-inferior area of superior antihelix crus.
Indications: lumbago, tinnitus, neurasthenia, nephropyelitis, enuresis, menopathy, impotence, etc.
10. Liver: posterio-inferior area of cymba concha.
Indications: hypochondriac pain, dizziness, premenstrual syndrome, irregular menstruation, hypertension, myopia, etc.
11. Spleen: posterio-superior area of the cavum concha.
Indications: adominal distension, diarrhea, constipation, anemia, leukorrhagia, Meniere’s disease, etc.
12. Heart: central depression of the cavum concha.
Indications: heart disease, neurasthenia,stomatoglossitis, etc.
13. Lung: peripheral to the heart area.
Indications: cough, chest distress, hoarseness, skin pruritus,urticaria, withdrawal syndrome, etc.
14. Endocrine: anterio-inferior area of the cavum concha medial to the intertragic notch.
Indications: dysmenorrhea, irregular menstruation, menopause syndrome, acne, hyper-thyroidism, etc.
15. Eye: center of the frontal surface of earlobe.
Indications: eye disease such as acute conjunctivitis, etc.
16. Cheek: between the eye and internal ear of the frontal surface of earlobe. Indications: facial paralysis, facial spasm, acne, mumps, etc.
5.6.4 Clinical Applications of Auricular Points
5.6.4.1 Indications for Ear Acupuncture
Ear acupuncture therapy incorporates a wide-range of indications and it is an effective, economical and simple technique withoutside effects. The indications of ear acupuncture therapy are as follows:
1. Pain Diseases: Various sprains and bruises, headaches, neuropathic pains, etc.
2. Inflammatory and Infectious Diseases: For example, pharyngitis, tonsillitis, mumps, cholecystitis, colitis, etc.
3. Dysfunctional Diseases and Allergic Diseases: For example, vertigo, hypertension, neurasthenia,urticaria, asthma, rhinitis, etc.
4. Endocrine Diseases and Metabolic diseases, diabetes mellitus, menopausal syndrome, hyperthyroidism, hypothyroidism, etc.
5. Miscellaneous: Auricular acupuncture is effective for inducing lactation and labor and for preventing and treating transfusion and infusion reactions. It is also widely used for cosmetology, drug withdrawal, age retardation and for the prevention of diseases and health care maintenance.
5.6.4.2 Auricular Point Selection Principle
1. Point selection according to the affected Area.
2. Point selection according to the differentiation of syndromes based on the theory of the zang-fu organs.
3. Point selection according to the differentiation of syndromes based on meridian theory.
4. Point selection according to the modern medical theory.
5. Point selection according to clinical experience.
5.6.4.3 Manipulation Method
1. Filiform Needling (Hao zhen fa): Characteristics differentiating it from the filiform needle therapy: a. Strict disinfection (iodine); b. Select no. 26-30, 0.3-0.5 cun needle and twist and rotate it merely when penetrate into the skin. The deep is enough for the needle to stand erectly without shaking. Needles are usually retained for 15-30 minutes, but in cases with chronic seizures or pain diseases, needles may be retained for longer periods.
2. Needle Embedding Therapy (Mai zhen fa): This therapy is conducted by embedding intradermal needles into auricular points. It is suitable for chronic and pain diseases. The therapeutic effect of the continuous stimulation consolidates the treatment, which can prevent relapses.
3. Auricular Seed Pressing Therapy (Ya wan fa): This therapy incorporates pressing adhering seeds onto the auricles to stimulate the points continuously. It is the most common therapy.
5.6.4.4 Precaution
1. Strict disinfection measures should be employed before doing acupuncture. Needling is contraindicated on areas where trauma or inflammation is present. If redness or swelling on a puncture hole is present after acupuncture, a 2.5% iodine tincture should be applied immediately to avoidsuppurativeperichondritis.
2. When treating sprains and motor disabilities, ask patients to move their affected extremities after insertions to enhance the therapeutic effects.
3. Needling is contraindicated with pregnant women.
4. Auricular acupuncture is inadvisable for cases with severe structural disease or serious anemia. Also, strong stimulation is not suitable for those with severe heart disease or hypertension.
5. Prevent needle fainting.